Fucoidan from brown seaweeds is known to contain multiple human defense functions. It maintains intestine health, which is normalized by the immune system. Fucoidan is the human defense function that is normalizing the intestinal system, making it indispensable for people’s health in these modern times. It also has biological effects of blood coagulation suppression, antitumor, blood rise suppression, triglyceride suppression, anti-allergic, and liver function improvement effects.
Thus, I would like to share the following study with you, “High Molecular Weight Fucoidan Restores Intestinal Integrity by Regulating Inflammation and Tight Junction Loss Induced by Methylglyoxal-Derived Hydroimidazolone-1,” by Jae-Min Lim et al. Studies show that dAGEs can damage the intestinal barrier by increasing intestinal permeability.
This study showed that when AGEs bind to AGE receptors (RAGE), the AGE/RAGE axis can activate intracellular pathways to promote oxidative stress by generating reactive oxygen species (ROS) and cell damage leading to inflammation. In particular, structural features of MG-H1 that bind strongly to RAGE may contribute to Inflammatory Bowel Disease (IBD).
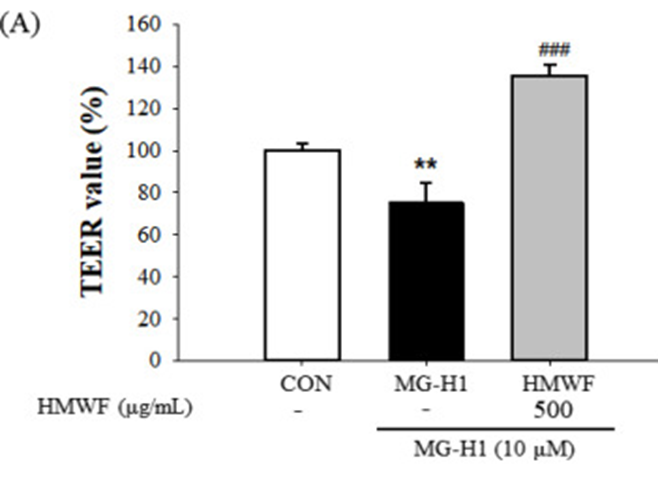
Immunomodulatory activity of High Molecular Weight Fucoidan (HMWF) from U. pinnatifida was reported. However, the neuroprotective activity against intestinal barrier disruption by MG-H1 has not been studied. The study investigated the ability of HMWF to repair intestinal damage caused by the MG-H1/RAGE axis in intestinal epithelial cells and animal models. HMWF + MG-H1 treatment reduced the number of reactive oxygen species generated by MG-H1 alone by 16.8%. Also, the study measured transepithelial electrical resistance (TEER) to assess the protective effect of HMWF against intestinal barrier dysfunction induced by MG-H1 treatment in differentiated Caco-2 cell monolayers. (See Figure 2A) Cells treated with MG-H1 showed a significant (p < 0.01) reduction in Caco-2 monolayer integrity compared to untreated control cells, as TEER values were reduced relative to control values. However, TEER values after HMWF + MG-H1 treatment were significantly (p < 0.001) increased compared to MG-H1 treatment, preserving the monolayer integrity of Caco-2 cells. (See Figure 1A )
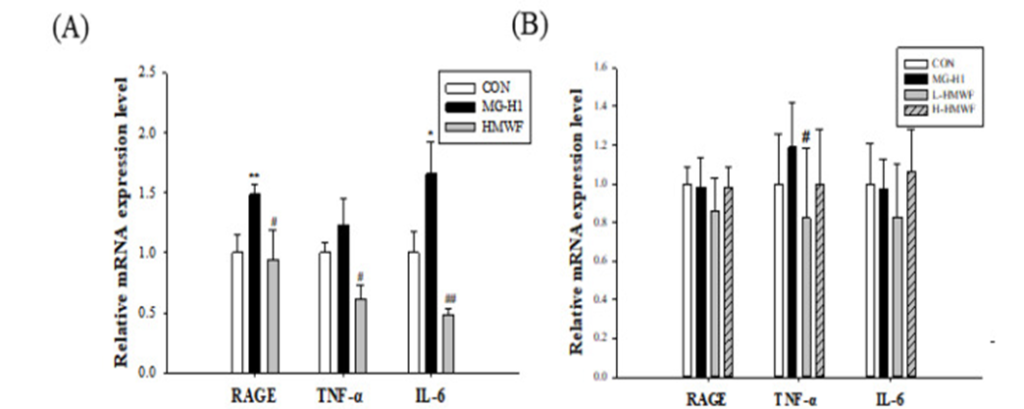
The research determined the effect of HMWF on inflammation induced by MG-H1 in Caco-2 cells and mouse colon; proinflammatory cytokine expression was measured at the mRNA level. Expression of interleukin-6 (IL-6) and tumor necrosis factor (TNF-α) was higher in MG-H1-treated cells than in control cells, with the former significantly increased. (See Figure 2A) However, combined MG-H1 + HMWF-treated cells exhibited lower levels of cytokines than MG-H1-treated cells and even lower than control cells. Mouse colon tissue shows increased TNF-α expression in the MG-H1 treated group compared to the control group. (See Figure 2B) On the other hand, oral treatment with HMWF significantly reversed the elevation of TNF-α caused by intravenous infusion of MG-H1. As a result, HMWF treatment can suppress the increased proinflammatory cytokine expression seen in Inflammatory Bowel Disease.
Additionally, HMWF treatment prevented MG-H1-induced expression of tight junction markers, including zonule obliterans-1, occludin, and claudin-1 in Caco-2 cells and mouse colonic tissue at the mRNA and protein levels. HMWF also plays an essential role in preventing AGEs receptor (RAGE)-mediated intestinal injury in Caco-2 and MG-H1-treated mice. Finally, HMWF inhibited the activation of nuclear factor kappa B and its target genes that cause intestinal inflammation. Hence, these results suggest that cost-effective HMWF may be essential in preventing intestinal barrier dysfunction induced by AGEs.
Source: Mar Drugs. 2022 Sep; 20 (9): 580 doi: 10.3390/md20090580
