The purpose of this blog is to shed light on a study that delved into the effects of low-molecular-weight fucoidan (LMF) as a supplement to neoadjuvant on the quality of life (QoL) and clinical outcomes of patients diagnosed with locally advanced rectal cancer (LARC). The study, “The Auxiliary Effects of Low-Molecular-Weight Fucoidan in Locally Advanced Rectal Cance Patients Receiving Neoadjuvant Concurrent Chemoradiotherapy Before Surgery: A Double-Blind, Randomized, Placebo-Controlled Study” by Hsiang-Lin Tsai et al. The research findings indicate that the primary objective of the study was to assess how the inclusion of LMF as an adjunct to neoadjuvant treatment influenced the quality of life (QoL) and clinical outcomes of patients diagnosed with LARC.
The Ministry of Health and Welfare in Taiwan has released data indicating that colorectal cancer has been the most prevalent form of cancer in the country since 2006. This highlights the significance of addressing treatment strategies for colorectal cancer as a crucial topic. Neoadjuvant CCRT followed by surgical resection is the standard treatment for LARC located in the mid or lower rectum. CCRT administration may induce some AEs (advanced effects) and reduce QoL.
Initially, there were a total of 87 patients, with 44 in the fucoidan group and 43 in the placebo group, included in the study. The researchers analyzed the impact of treatment on quality of life scores and clinical outcomes, examining data before treatment and at 1, 2, and 3 months after treatment. Moreover, they examined alterations in gut microbiota before and after the treatment.
Prior to receiving treatment, a comparison was made between the fucoidan group and the placebo group in terms of the scores on eight health-related quality of life scales derived from The Functional Assessment of Cancer Therapy for Patients with Colorectal Cancer (FACT-C). Quality of life scores in both groups remained unchanged after treatment, and there were no notable differences observed. At 2 months and 3 months after treatment, the mean score of the fucoidan group showed a significant difference compared to the mean score of the placebo group, while analyzing the results for the placebo group at 1 month, 2 months, and 3 months after treatment.
The study divided DFS and OS into two groups. DFS was defined as the time from randomization to tumor recurrence or death, while OS was defined as the time from randomization to death or the last date of follow-up. While there were no notable distinctions among the groups, it seems that the fucoidan group shows a tendency towards improved overall survival (OS) but not improved disease-free survival (DFS). The 2-year DFS in the fucoidan and placebo groups was 86% and 76%, respectively. DFS over three years was 80% and 76%, respectively. The 2-year OS of the fucoidan group and the placebo group was 100% and 91%, respectively, while the 3-year OS was 96% and 83%, respectively. Hence, it is necessary to have a lengthier follow-up period in order to determine if there is a relationship between fucoidan administration and better DFS and OS.
In addition, comparing the incidence of two AEs was significantly lower in the fucoidan group than in the placebo group (skin rash/itch: 0% vs 9.3%, P = .038; fatigue: 75.0% vs 95.3%, P = .008). The most common serious AEs in the fucoidan group were neutropenia (2.3%) and anemia (2.3%), and the most common serious AE (grade III or higher) in the placebo group was neutropenia (6.9%).
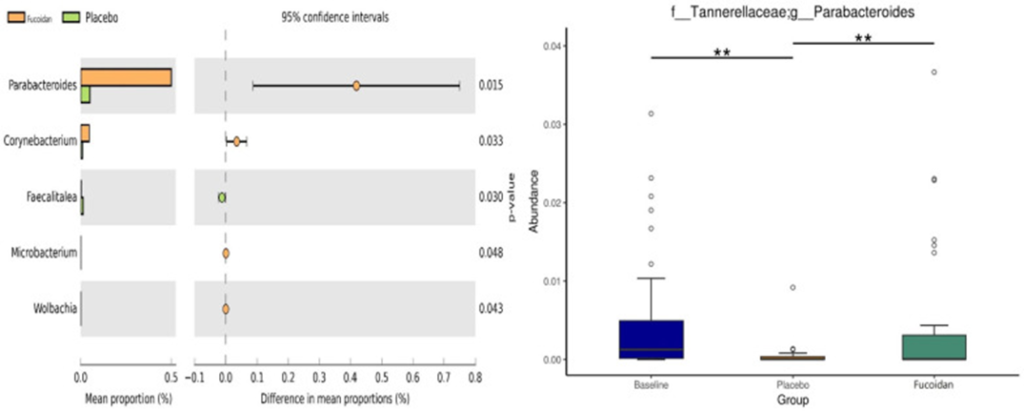
Furthermore, the examination of the pre- and post-treatment gut microbiota in both groups revealed that the genus Parabacteroides exhibited the most significant variation, as shown in Figure 1. The only known effects of Parabacteroides distasonis are beneficial in the context of colorectal cancer. According to multiple studies, there is a negative correlation between the amount of P. distasonis in the stool and the occurrence of intestinal tumors.
This study has some limitations. Firstly, while this study is prospective and double-blind, having a larger sample size would have bolstered the confidence in the findings. Secondly, certain patients were not included in the study due to incomplete preoperative CCRT and being untraceable for over a year. Thirdly, the inadequate length of the follow-up period prevented a thorough evaluation of the treatment’s long-term effectiveness, particularly in terms of overall survival (OS).
However, this trial is unique as it is the first to employ a prospective, randomized, double-blind, placebo-controlled methodology to examine the efficacy of LMF as a complementary therapy for individuals with LARC. Many studies have shown that LMF has anti-cancer properties and could be a promising treatment for cancer. The study demonstrated the benefits of LMF in improving QoL, especially in PWB, fatigue, skin itching, and increasing Parabacteroides microbial levels during the CCRT period. This study can provide valuable insights for the development of cancer treatments, particularly those that combine chemotherapy and radiotherapy.
Source: Integr Cancer Ther. 2023; 22: 15347354231187153. doi: 10.1177/15347354231187153
