A glioma is a tumor of glial cells (glia) that make up the brain. It is classified as benign glioma, which grows slowly. It has a relatively straightforward border with the adjacent normal part and malignant glioma, which multiplies, invades the adjoining region, and has an unclear edge. According to the WHO classification determined by pathological examination, malignant gliomas fall under grades 3 and 4, divided into four stages. Malignant glioma (MG) is a brain tumor with a poor prognosis and is known to recur after multimodality therapy. MG prediction remains poor despite many advances in surgery, radiation, and chemotherapy. Thus, finding more effective treatments that don’t cause side effects is imperative.
On a positive note, there is already a solution available. A natural product known as fucoidan, extracted from brown algae, has no side effects. It has several biological activities, including anticoagulant, antioxidant, immunomodulatory, anti-inflammatory, antibacterial activity, and antitumor properties.
Therefore in this blog, I would like to share the study “Epigenetic Modification and Differentiation Induction of Malignant Glioma Cells by Oligo-Fucoidan” by Chien-Huang Liao et al.
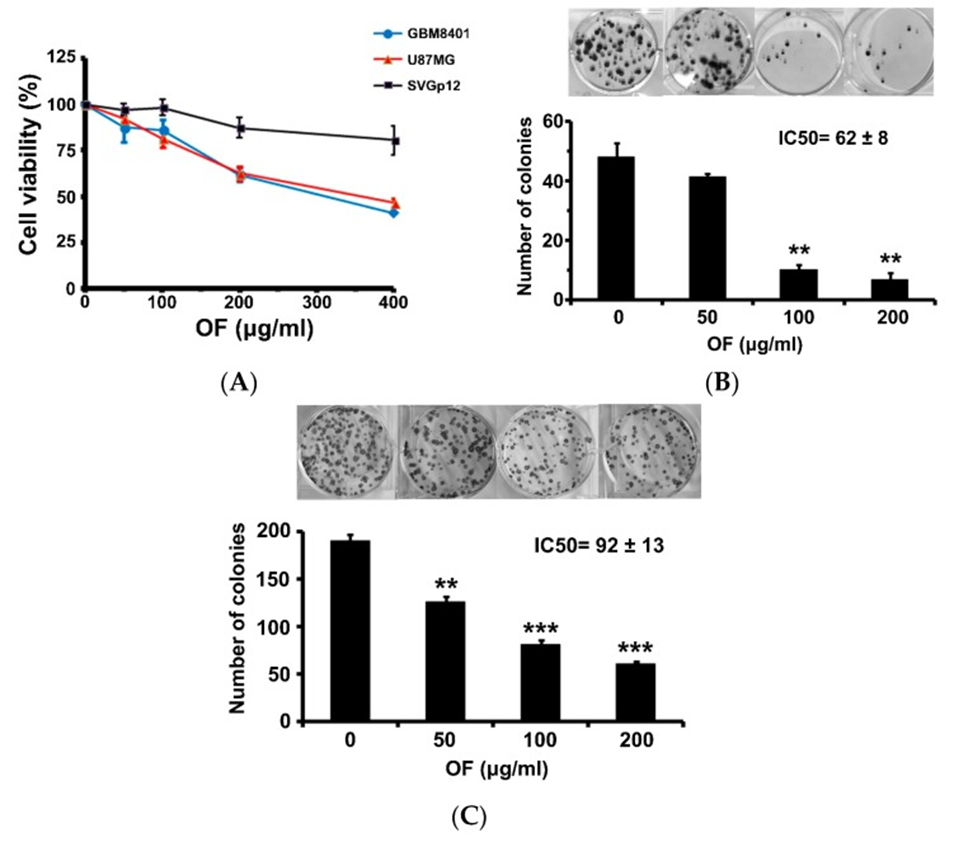
Researchers first investigated the effect of brown algae (Laminaria japonica) derived oligo-fucoidan (OF) on this concept in MG cells, including grade III U87MG cells and grade IV glioblastoma multiforme (GBM) 8401 cells, immortalized astrocyte SVGp12 cells and also compared them. Later, they investigated the effect of OF on the proliferation of human MG cells (GBM8401 and U87MG) as determined by the sulforhodamine (SRB) assay. Varying degrees of growth inhibition was observed after 72 h exposure to OF. At a 400 μg/mL concentration, cell proliferation of GBM8401 and U87MG cells was suppressed to 40% and 46% of control, respectively. (See Figure 1A)
In contrast, OF had only a slight inhibitory effect on the proliferation of immortalized astrocyte SVGp12 cells at the same concentration, suggesting preferential suppression of cancer cells by OF. At a 200 μg/mL concentration, OF significantly reduced colony formation of GBM8401 and U87MG cells by 14% and 32%, respectively. (See Figure 1B, C)
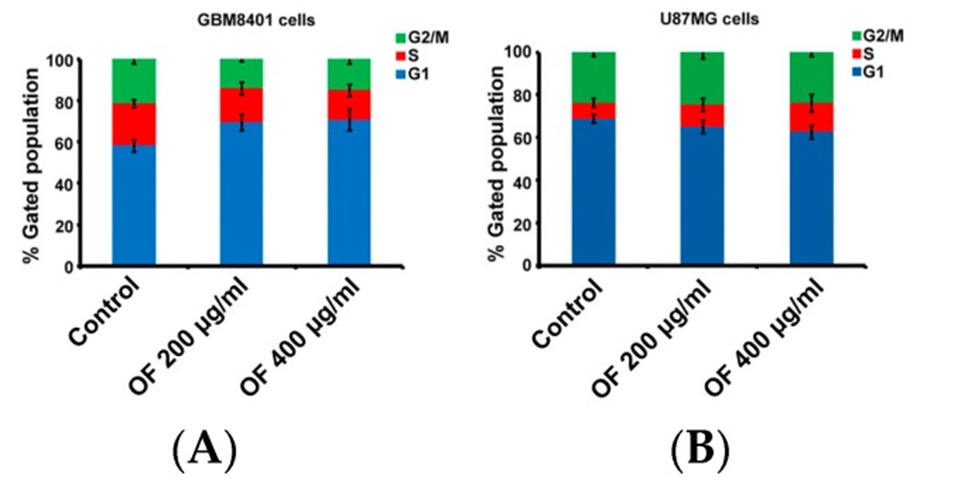
Next, figures 2A and B show the cell cycle distribution of GBM8401 and U87MG cells after treatment with OF at 200 and 400 µg/mL concentrations for 72 hours. OF caused cell cycle arrest in GBM8401 cells by increasing the percentage of the G1 phase from 58% (control) to 69% and 71%, respectively. (See Figure 2A) In U87MG cells, the S phase increased from 7% (control) to 10% and 14%, depending on the OF concentration. (See Figure 2B) The results demonstrate that OF can inhibit proliferation by arresting the cell cycle at the G1 or S phase in different MG cells.
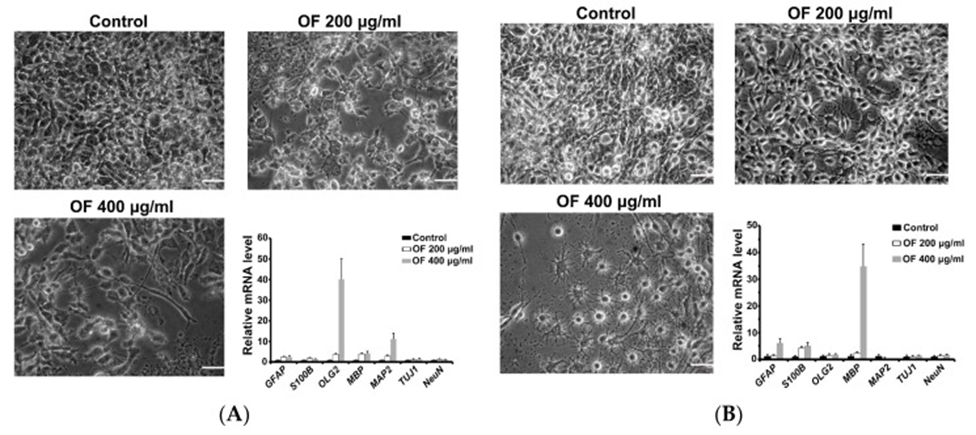
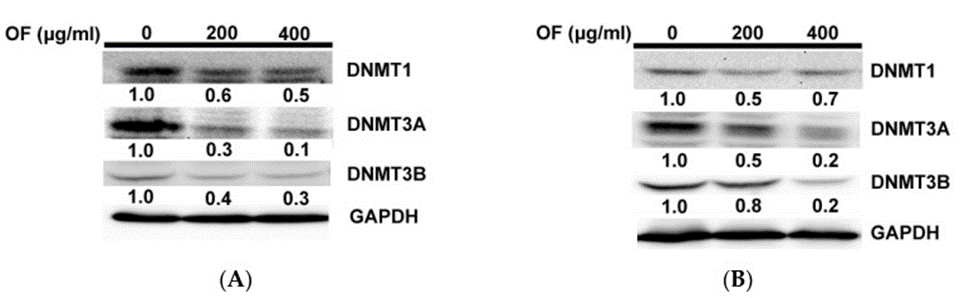
And they investigated the molecular mechanisms underlying the differentiation of OF-treated MG cells. Previous studies have found that OF can induce miR-29b, suppressing her DNMTs (DNMT1, 3A, and 3B) in cancer cells. Thus suggesting that DNMTs in MG cells are inhibited during OF-induced differentiation—deciding whether or not. OF suppressed protein levels of DNMTs in both GBM8401 (See Figure. 4A) and U87MG (See Figure. 4B) cells. Epigenetic mechanisms may be essential in OF-induced differentiation, including DNA demethylation.
These results show that OF significantly suppressed the proliferation of MG cells and only marginally affected the proliferation of SVGp12 cells. OF increased DNA methyltransferases 1, 3A, and 3B with clear mRNA induction of differentiation markers in U87MG and GBM8401 cells protein expression. Thus, methylation of p21, a DNMT3B target gene, was decreased by OF. Additionally, they found that combining with the clinical DNMT inhibitor decitabine and OF may synergistically affect growth inhibition and MBP induction in U87MG cells.
They believe Oligo-fucoidan (OF) has a benefit on Malignant Glioma Cells (MG) through the study. However, further adequate clinical trials are needed to evaluate the clinical benefits of MG once its efficacy in vivo is confirmed.
Source: Mar Drugs. 2019 Sep; 17(9): 525. doi: 10.3390/md17090525