The strong correlation between high-salt diets, defined as diets with excessive intakes of salt, and the development of a number of serious illnesses, including hypertension, chronic kidney disease, and various autoimmune diseases, is well established in the medical literature. However, the mechanisms underlying HSD-induced inflammation promotion and exacerbation of these diseases have not been fully elucidated.
In this blog, I would like to present the following study, “L-fucose and fucoidan alleviate high-salt diet-promoted acute inflammation” by Wenhua Li et al. The researchers observed that HSD intake reduced the amount of the gut microbial metabolite L-fucose, leading to a more pronounced inflammatory response in mice.
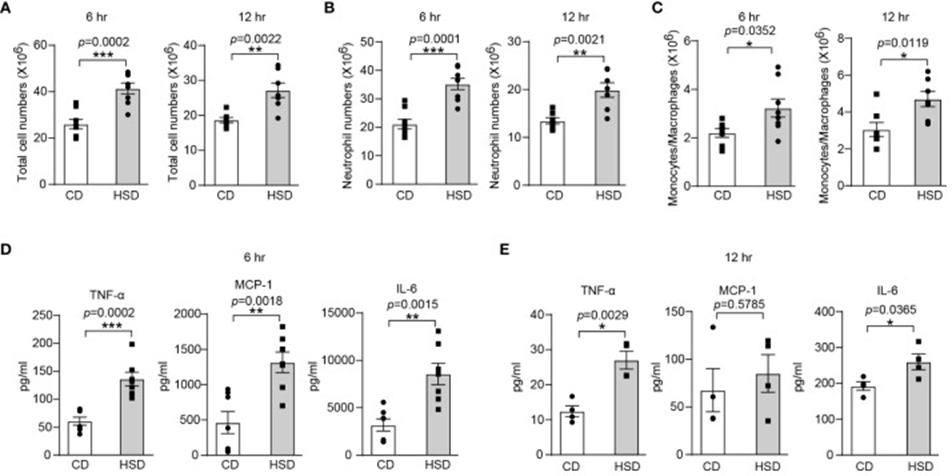
The study’s findings suggest a significant role for inflammation in HSD-related illnesses, with zymosan A shown to induce inflammation via macrophage and NF-κB activation. To investigate the inflammatory effects of HSD, they used a classical model of acute inflammation called peritonitis, induced by intraperitoneal injection of zymosan A. The model was characterized by the infiltration of inflammatory cells, especially neutrophils, and increased production of inflammatory molecules. The results of Figure 1 showed that after undergoing HSD, the total cell and neutrophil numbers in the peritoneal cavity were significantly increased, as were the levels of the inflammatory cytokines tumor necrosis factor-alpha (TNF-α) and interleukin 6 (IL-6). Additionally, monocyte chemotactic protein-1 (MCP-1, also known as C-C motif chemokine ligand 2 or CCL2). This data shows that consuming HSD promotes inflammation in an acute peritonitis model using zymosan A.
Following confirmation of HSD’s pro-inflammatory action in a zymosan A-induced peritonitis model, the study’s authors delved into the underlying mechanisms. First, they measured the Na+ concentration in the ascites supernatant at various time points. Biochemical analysis revealed that there was no significant difference in Na+ concentration between the HSD and CD groups. The findings suggest that HSD promotes inflammation through a mechanism independent of sodium accumulation within the peritoneal cavity. From this result, to verify that HSD may accelerate inflammation through an indirect mechanism such as regulating the gut microbiota, mice in both the HSD and CD groups were administered broad-spectrum antibiotics for 4 weeks to deplete the gut microbiota. The antibiotics’ effect on peritonitis recovery was examined following a course of antibiotic treatment.
Compared to no antibiotic treatment, antibiotic treatment (in both HSD and CD groups) increased levels of inflammatory cytokines like TNF-α. However, total cell counts, neutrophil and monocyte/macrophage infiltration, and expression of TNF-α, MCP-1, and IL-6 increased 6 and 12 hours after zymosan A injection. The results strongly support a role for gut microbiota dysbiosis in HSD-induced inflammation.
In order to thoroughly investigate and understand the impacts that HSD has on the gut microbiota, a comprehensive analysis of the diversity and composition of the fecal microbiota in mice was conducted using 16S rRNA sequencing techniques. The study revealed that eight weeks on a high-sugar diet resulted in a less diverse and rich gut microbiome and significantly altered the types of bacteria present.
Metabolomics analysis (LC-MS/MS) showed significantly lower L-fucose levels in the HSD group compared to the CD group. This reduction correlated strongly with HSD-induced alterations in gut microbiota. The potential impact of L-fucose on inflammation showed that the inflammatory response was significantly reduced in the L-fucose-treated mouse group. These findings suggest that L-fucose plays an important role in regulating inflammation in the context of HSD intake. Moreover, the researchers documented a reduction in the concentration of fucosidase—the enzyme that cleaves L-fucose from glycans—within the subjects classified as belonging to the HSD group, providing further insight into the underlying mechanisms.
This implies that HSD could decrease L-fucose production by lowering the levels of fucosidase-producing bacteria. The observed drop in L-fucose production might be pro-inflammatory, contrasting with L-fucose’s reported anti-inflammatory effects. L-fucose has also been found to inhibit MIF/MAF-induced priming of alveolar macrophages for oxidative burst. The study revealed that L-fucose treatment significantly reduced the release of IL-6 and MCP-1 in RAW264.7 cells from HSD-treated mice and PM from HSD-treated mice, suggesting that L-fucose can serve as a nutrient for the colonization of microorganisms such as bifidobacteria and alter the composition of the microbiota. Gut bacteria and L-fucose can together reduce DSS-induced colitis by managing bile acid metabolism. Furthermore, L-fucose can be utilized by various bifidobacterial species to form 1,2-propanediol, a precursor for intestinal propionate formation. The production of propionate may reduce intestinal inflammation. L-fucose shows promise as a therapeutic agent for reducing inflammation associated with HSD, based on these findings.
In the next phase of their research, the team performed a series of experiments using mice models to investigate and validate the anti-inflammatory effects of fucoidan against HSD-induced inflammation. They also observed that fucoidan reduced the acute inflammatory response of macrophages. They found that the effective dose of fucoidan was lower than that of L- fucose. This might be linked to sulfate, a major fucoidan component.
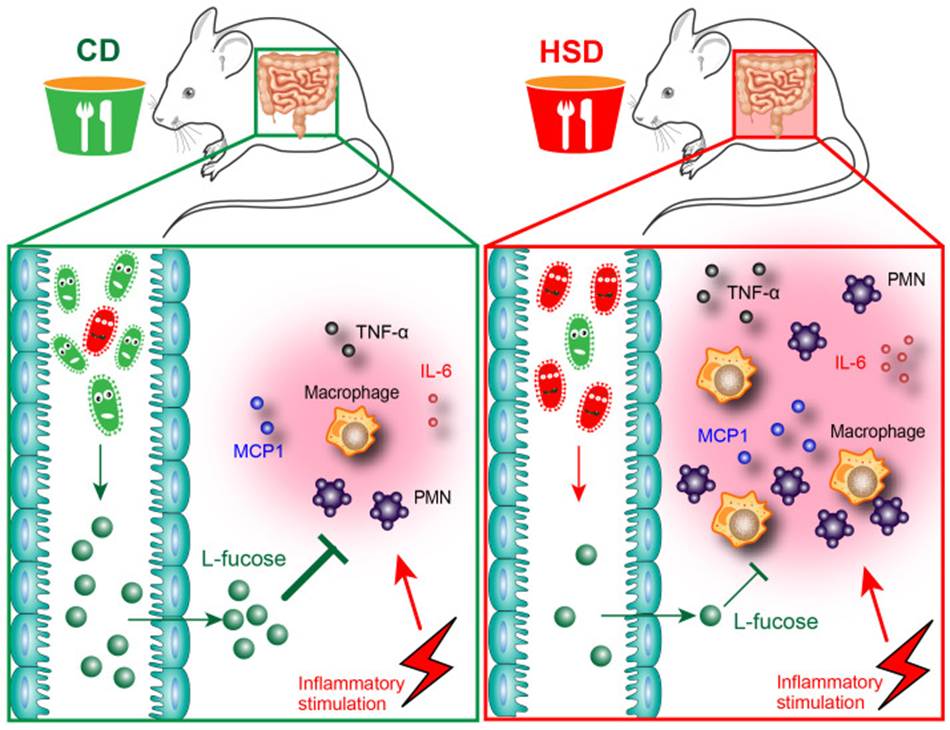
Additionally, the study demonstrated that HSD intake reduced gut microbiota diversity and richness, disrupting the composition of gut microbiota and metabolites, which play an important role in promoting peritonitis (Figure 2). In the case of zymosan A-induced peritonitis, both L-fucose and fucoidan showed a potential to lessen the inflammatory responses triggered by HSDs. This study sheds new light on the underlying mechanisms behind the pro-inflammatory effects of HSDs, and the identification of potential drug candidates such as L-fucose and fucoidan will pave new avenues for clinical treatment.
Source: Front Immunol. 2024; 15: 1333848. doi: 10.3389/fimmu.2024.1333848
