Diabetes has been reported to be associated with cancer development in the United States since 2010. People with diabetes have a 20% higher risk of cancer than individuals without diabetes. Primarily, it is twice as much for pancreatic and liver and 1.4 times for colorectal cancer. On the other hand, breast cancer and prostate cancer were not associated with diabetes.
In addition, insulin might be one of the main reasons diabetes is associated with the onset of cancer, which has been closely related to diabetes. When insulin, a hormone that lowers blood sugar levels, lacks its function, insulin concentration in the blood increases (hyperinsulinemia), and IGF-1 (insulin-like growth factor-1) increases to compensate for it. Insulin and IGF-1 are supposed to increase the risk of carcinogenesis in diabetes because they promote cell proliferation. Obesity and lack of exercise often cause hyperinsulinemia. Hence, a similar mechanism is considered for cancers strongly associated with obesity and lack of exercise.

So, in this blog, I would like to share the study “Fucoidan Structure and Its Impact on Glucose Metabolism: Implications for Diabetes and Cancer Therapy” by Blessing Mabate et al.
First, cancer cells can reprogram glucose metabolism. It is essential for their survival and progression. Tumor progression involves the uncontrolled proliferation of cells with enhanced energy-producing mechanisms to resist metabolic stress. Cancer cells can switch from oxidative phosphorylation (OXID-P) to glycolysis. Glycolysis produces two pyruvate molecules from the breakdown of a single glucose molecule.
After being converted to acetyl coenzyme A (acetyl-CoA), it is completely oxidized in the presence of oxygen (normal oxygen state), producing carbon dioxide and water through the Krebs cycle. Recent studies have also demonstrated the significance of the pathophysiology of glucose metabolism and the glycolytic flux in the development of tumors.
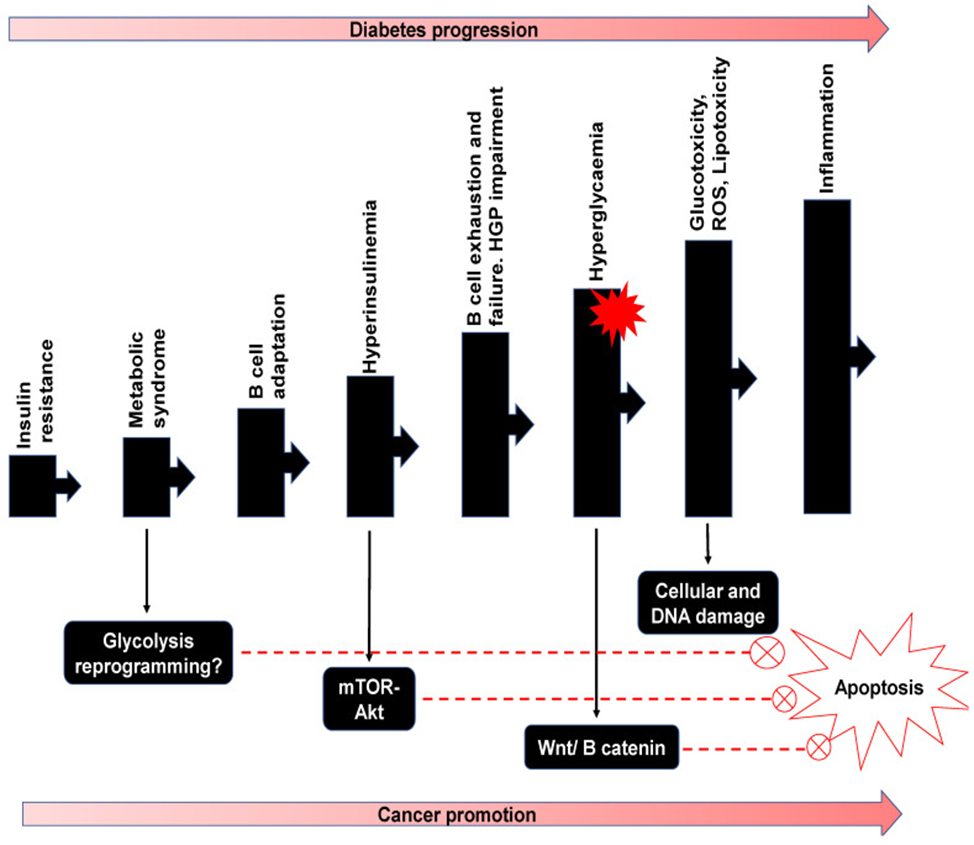
Epidemiological evidence shows that people with diabetes are at very high risk for multiple types of cancer. Recently, various pathways of diabetes have been reported to be associated with cancer progression. Tudzarova et al. reviewed the clinical association of type 2 diabetes with several cancers and highlighted the complexity of the association with diabetic cancer. (See Figure 1) Events that lead to type 2 diabetes include insulin resistance, pancreatic β-cell damage, and consequent changes in hepatic glucose production (HGP). The resulting hyperglycemia associated with overworked beta cells can lead to metabolic reprogramming and switching to glycolysis, which is a characteristic of cancer development.
Hyperinsulinemia is associated with stimulating insulin-like growth factor (IGF) and epidermal growth factor (EGF), which activate the mTor-Akt pathway. In addition to hyperglycemia, which cooperates with the Wnt / β-catenin pathway, inhibition of apoptosis can cause cell damage due to glucose toxicity and elevated reactive oxygen species (ROS). Furthermore, the cellular response to ROS can cause inflammation and work with mitogens and metabolic pathways to initiate or accelerate cancer progression. (See Figure 1)
Some common disease-progressing symptoms of diabetes and cancer include hyperinsulinemia, hyperglycemia, and inflammation. Therefore, the proposed focus is on glucose. Pathophysiology as a target for dual control and suppression of diabetes and cancer makes sense. As a result, fucoidan may be applied to this therapeutic effort and other similar therapeutic compounds.
Recent studies have also established that fucoidan increases insulin sensitivity, lowers postprandial blood glucose levels, and prevents hyperglycemia in vivo. In addition, fucoidan is involved in activating pathways that increase insulin production and even translocate glucose transporter molecules. Therefore, fucoidan seems to be therapeutically valuable for preventing the tumor from diabetes.