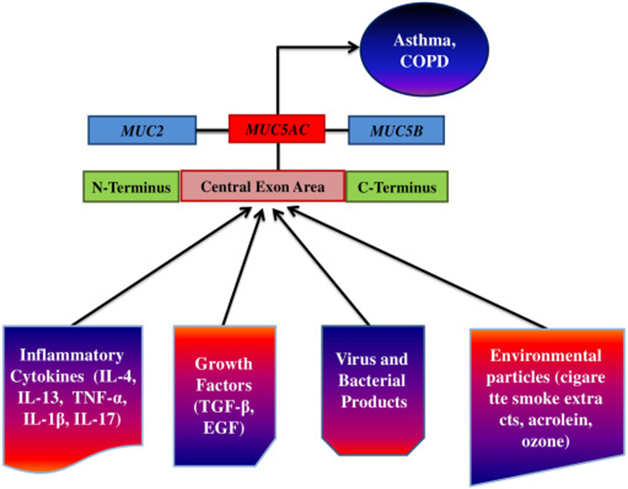
Excessive mucus production is characteristic of the etiology of several airway diseases, including chronic bronchitis, asthma, and cystic fibrosis.
The MUC5AC and MUC5B proteins are significant components of the human mucus layer and contribute to airway mucus’s barrier function and rheology. MUC5AC is upregulated in the airways during various airway disorders such as COPD, CF, and asthma.
Therefore, in my current blog, I would like to share how fucoidan can affect the treatment of chronic respiratory diseases with the relationship between fucoidan and MUC5AC based on “Inhibition acrolein-stimulated MUC5AC production by fucoidan in a human bronchial epithelial cell ” by Yuba Raj Pokharel et al.
It’s essential to know that acrolein is an intense, electrophilic, and volatile liquid produced by various natural and synthetic processes, including the complete combustion of organic materials such as fuels and tobacco. In addition, patients treated with the anticancer drug cyclophosphamide are frequently exposed to the metabolite acrolein.
Unfortunately, smoking is associated with various respiratory illnesses, including chronic obstructive pulmonary disease (COPD), as tobacco chlorine production is relatively high (50-70 ppm). In addition, both acrolein and tobacco smoke extract stimulate mucin secretion from bronchial epithelial cells.
So then examined whether acrolein stimulates MUC5AC expression in NCI-H292 cells (human airway epithelial cell) by Reverse transcription-polymerase chain reaction (RT-PCR) analysis.
The analysis showed that fucoidan inhibits MUC5AC expression and protein secretion in cells stimulated with acrolein, a toxic aldehyde present in tobacco smoke.
It is now known that fucoidan is a marine sulfated polysaccharide with antiviral, antiangiogenic, antitumor, contraceptive, antithrombotic, anticoagulant, and anti-inflammatory properties. In addition, a study recently reported that high concentrations of fucoidan (10-100 mg/ml) inhibit iNOS expression and subsequent nitric oxide production in activated macrophages. However, the effect of fucoidan on bronchial mucin secretion has not been elucidated yet.
The study evaluated that fucoidan inhibits the acrolein-mediated expression of MUC5AC by blocking AP-1 activation in NCI H292 cells, a human bronchial epithelial cell line.
They first determined whether acrolein stimulates MUC5AC on expression in NCI-H292 cells. Acrolein 0.3 and 1 ng / ml significantly increased MUC5AC mRNA. However, MUC5AC was not induced at high concentrations of Acrolein (> 3 ng / ml), probably due to the cytotoxicity of acrolein.
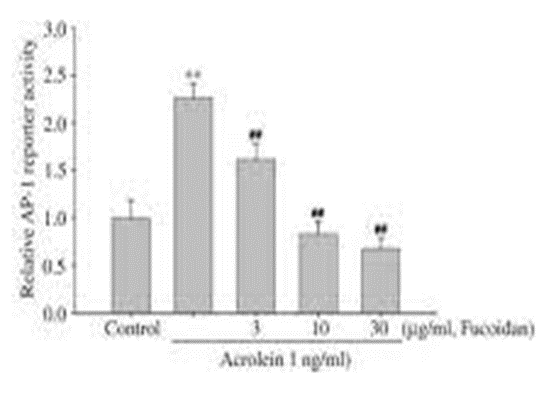
They further measured the inhibitory effect of fucoidan on AP-1 activity (to regulate gene expression in response to various stimuli) since MUC5AC transcription via acrolein depends on AP-1 activation. Fucoidan (30 or100 mM) significantly inhibited the acrolein-induced increases in AP-1 reporter activity (Fig. 1). So, these results support the idea that fucoidan may block AP-1 activation and inhibit MUC5AC expression. A similar mechanism stops the induction of nitric oxide synthase in activated macrophages.
Fucoidan suppressed acrolein-induced MUC5AC expression in human bronchial epithelial cells through inhibition of AP-1 activation. Since the significant pathological markers of asthma and COPD are chronic inflammation and mucin production, fucoidan may have potential treatment for chronic respiratory illness.