Radioactive iodine (RI) plays a crucial role in thyroid cancer treatment by eliminating any leftover cancer cells and lowering the risk of the disease returning. Although RI is known for affecting the thyroid, the most prevalent consequence is the deterioration of the salivary glands, causing discomfort and enlargement. Subsequently, the ingestion of RI leads to xerostomia, oral discomfort, taste disorder, and difficulty in eating. RI treatment can be uncomfortable for patients and may even hinder the successful treatment of thyroid cancer.
In this blog, I would like to share the following study with you: “Fucoidan attenuates radioiodine-induced salivary gland dysfunction in mice” by Young-Mo Kim et al.
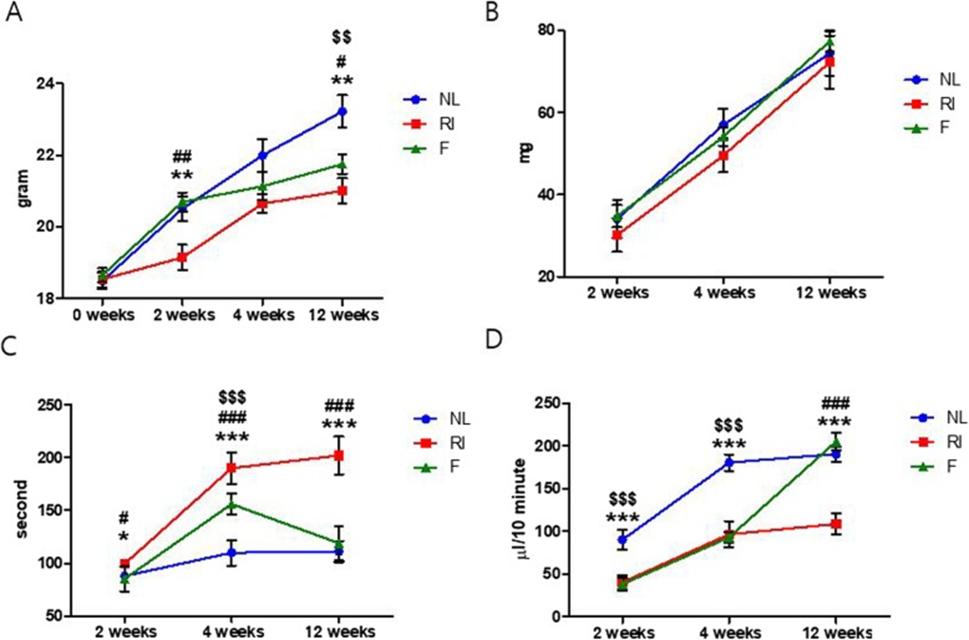
The female C57BL/6 mice were initially separated into three distinct groups: i) normal (control), ii) RI-treated, and iii) fucoidan and RI-treated. Mice from each group were divided into three subgroups, and salivary flow and lag time measurements. When the experiment began, the groups had comparable body weights, indicating no significant differences. However, after the experiment, the body weight of the mice in the RI group was significantly lower than that of the mice in the normal control group and the mice in the fucoidan group. The results displayed in Figure 1a demonstrate a substantial increase in body weight among the mice in the RI group compared to the mice in the RI group, a difference that was statistically significant at both 2 and 12 weeks post-treatment. Although the RI group demonstrated a trend of lower gland weights compared to the normal and fucoidan groups at 2, 4, and 12 weeks following RI, these differences did not reach statistical significance, as depicted in Figure 1b.
Following the administration of RI, significant differences in lag time were observed between the groups at 2, 4, and 12 weeks post-treatment, as illustrated in Figure 1c. The lag time in the normal group was lower than that of the RI group at 2, 4, and 12 weeks. At 4 and 12 weeks after RI, the lag time in the fucoidan-administered group was lower than that of the RI group. Also, the salivary flow rate in the normal group was higher than that of the RI and fucoidan groups. Two weeks following radiation injury (RI), the salivary flow rate of the group treated with fucoidan had returned to the same level as the group that had not received radiation, as illustrated in Figure 1d.
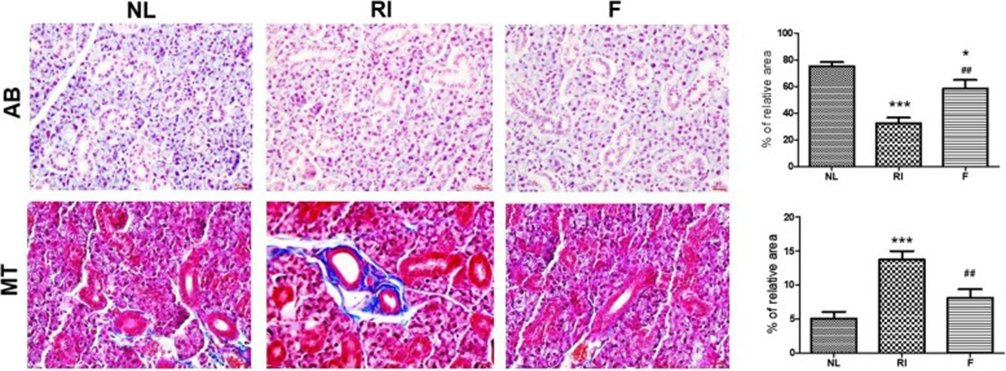
The next steps involved examining histological changes and conducting apoptosis assays. Histological changes in SGs were visualized by H&E, AB, and MT staining at 12 weeks after RI. Morphometric analysis of AB staining, which represents mucin density, showed that mucin production was decreased in the RI group compared with the normal group. However, mucin was significantly increased in the fucoidan group compared with the RI group. MT staining to examine fibrosis showed that the degree of fibrosis was the highest in the RI group compared with the normal group, whereas the fucoidan group had a lower level of fibrosis compared with the RI group. (See Figure 2)
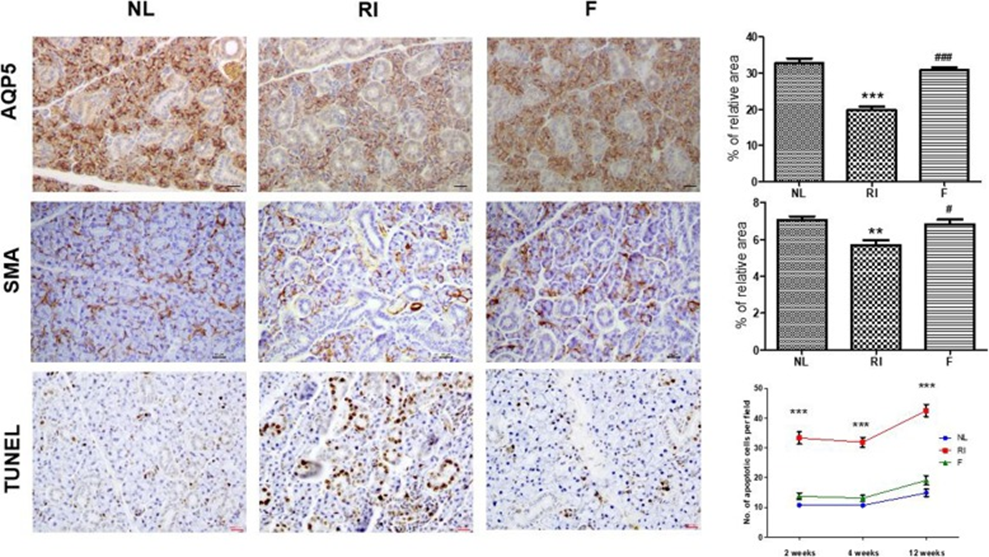
The cytoprotective effect of fucoidan on salivary epithelial cells and myoepithelial cells was evaluated by immunohistochemical staining. As shown in Figure 3, the expression of AQP5 (a marker for salivary epithelial cells) and α-SMA (a marker for myoepithelial cells) was decreased in the RI group compared with the normal group. Fucoidan treatment increased the staining intensity of these cells compared with the RI group, suggesting that fucoidan can protect salivary epithelial cells and myoepithelial cells from RI-induced cytotoxicity. TUNEL assay showed that the number of TUNEL-positive cells was significantly higher in the RI group and significantly lower in the fucoidan group. The increase in MMA score at 2, 4, and 12 weeks after RI compared with the control group was more significant than that in the control group, 10.8 ± 0.7, 10.7 ± 0.6, and 14.9 ± 1.2, respectively.
Single photon emission computed tomography (SPECT) revealed alterations in salivary 99mTc pertechnetate parameters. The study showed that the radiation-induced (RI) group had reduced 99mTc pertechnetate excretion 12 weeks after radiation exposure, while the fucoidan group regained their excretion ability comparable to the normal control group.
While more research is required to fully understand how fucoidan works, it has shown promise in fighting thyroid cancer by stopping cell growth, triggering cell death, and limiting blood vessel formation in cancerous cells. This finding suggests that fucoidan administration can selectively protect SGs from RI-induced damage without adversely affecting the treatment of thyroid cancer.
Pre-treatment with fucoidan before radioactive iodine exposure has been shown to reduce radiation-induced salivary gland damage in mice. This suggests that fucoidan might be useful in preventing salivary gland dysfunction in thyroid cancer patients undergoing radioactive iodine therapy.
Source: BMC Oral Health. 2019; 19: 198. doi: 10.1186/s12903-019-0894-2
