Hypoxia is the condition of inadequate oxygen supply in body tissues, which can be local or systemic. It involves a decrease in vital signs such as activity tolerance and consciousness level. The artificially induced hypoxic condition, known as artificial hypoxia, can lead to the lethality of cancerous cells by depriving them of oxygen. Hence, Hypoxia induces epithelial-mesenchymal transition (EMT) through hypoxia-inducible factor 1α (HIF-1α) in various types of cancer, including gastric cancer, hepatoblastoma, pancreatic cancer, colon cancer, and breast cancer. EMT is an important process in cancer metastasis. The process of EMT involves epithelial cells losing cell polarity and cell-cell adhesion, while acquiring migratory and invasive properties, ultimately resulting in the formation of mesenchymal stem cells. To complete the metastatic process, cancer cells must migrate from the primary tumor. Studies on breast cancer have shown that the EMT phenomenon increases cancer cell migration and invasion and is closely associated with tumor development, invasion, and distant implantation. Also, HIF-1α levels in breast cancer tissues are associated with pathological stages, and higher HIF-1α levels may lead to higher proliferation rates and more aggressive tumor formation.
The presence of metastasis in triple-negative breast cancer (TNBC) leads to an unfavorable prognosis and high mortality rates due to the lack of effective treatment. Fucoidan is a complex sulfated polysaccharide extracted from wakame seaweed. Earlier investigations have revealed that it possesses anti-tumor effects in diverse cancer types. Although fucoidan has been found to have an impact on TNBC metastasis, there is still a need to determine its underlying mechanisms for further clarification.
Thus, in this blog, I would like to share the summary of the study, “Fucoidan inhibits epithelial-to-mesenchymal transition via regulation of the HIF-1α pathway in mammary cancer cells under hypoxia” by Weiwei Li et al.
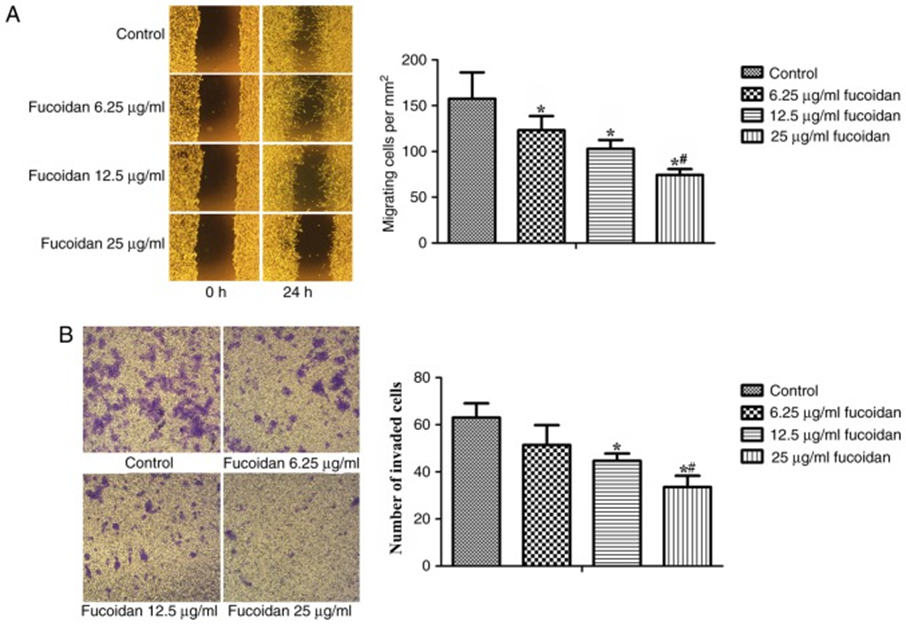
The study investigated the effect of fucoidan on epithelial-mesenchymal transition (EMT) in human triple-negative breast cancer (TNBC) cell lines in a hypoxic microenvironment. MDA-MB-231 human breast cancer cells were subjected to both Transwell assays and wound-healing assays to analyze their invasion and migration abilities, respectively. They detected whether fucoidan intervention had any effect on the EMT of MDA-MB-231 cells. As shown in Figure 1A, fucoidan treatment reduced the migratory ability of breast cancer cells. The inhibition of cell invasion was also observed after a 24-hour treatment with fucoidan at concentrations of 12.5 or 25 μg/ml. (See Figure 1B)
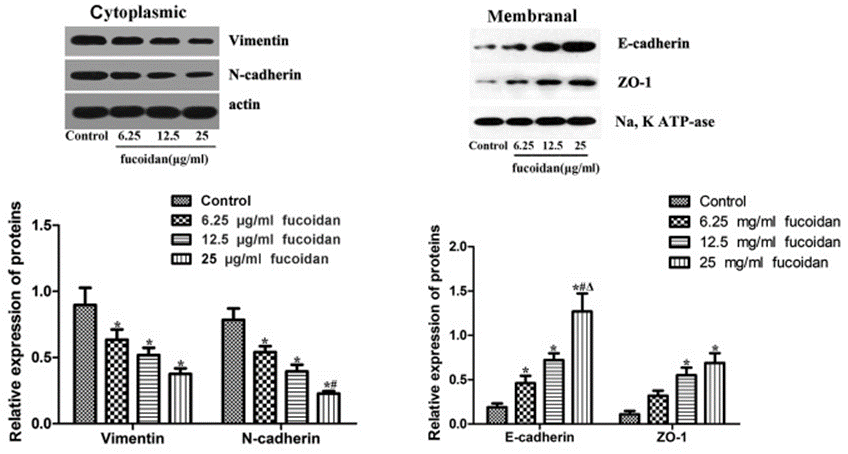
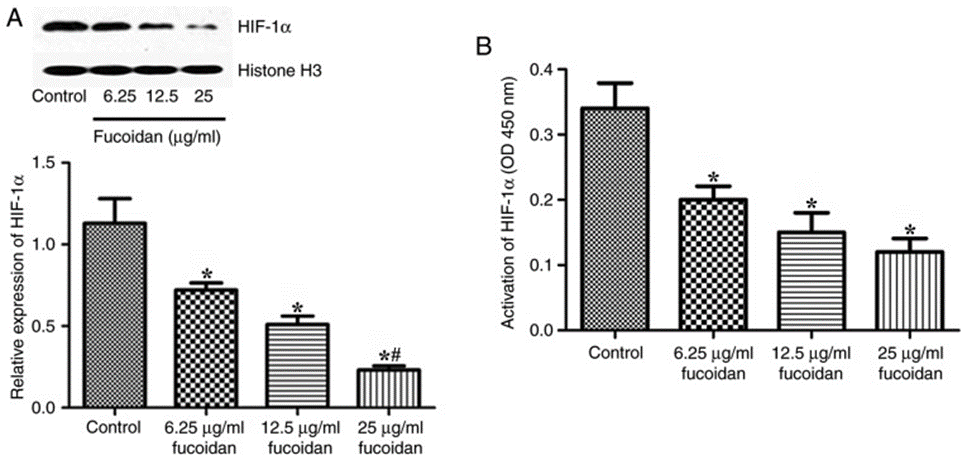
Fucoidan affects the expression levels of EMT markers. The results revealed that fucoidan treatment down-regulated the expression levels of mesenchymal markers N-cadherin and vimentin. (See Figure. 2) The epithelial markers ZO-1 and E-cadherin were barely expressed in the membrane of MDA-MB-231 cells, whereas fucoidan treatment significantly increased the expression levels of ZO-1 and E-cadherin. Inhibition of nuclear protein accumulation and HIF-1α activation is caused by Fucoidan. Expression levels of EMT markers and hypoxia-inducible factor 1α (HIF-1α) were detected by Western blotting. Nuclear protein levels of HIF-1α decreased after treatment with fucoidan under hypoxic conditions. (See Figure. 3A) HIF-1α activation was also assessed.
HIF-1α activation was reduced as a consequence of fucoidan treatment, as demonstrated in Figure 3B. Under hypoxia, fucoidan treatment suppressed the proliferation of breast cancer cells. Fucoidan also down-regulates the expression of HIF-1α target genes. HIF can regulate the expression of several genes involved in tumor growth, metastasis, and metabolic reprogramming. HIF-1α can directly or indirectly regulate the EMT regulators TWIST, Snail, CAIX, and GLUT-1. Expression levels of TWIST, Snail, CAIX, and GLUT-1 were detected by Western blotting. Expression levels of TWIST-1, Snail, CAIX, and GLUT-1 were inhibited after treatment with fucoidan.
Overexpression of HIF-1α results in the reversal of fucoidan-mediated suppression of cell migration and invasion. We transfected MDA-MB-231 cells with a HIF-1α overexpression plasmid (HIF-1α-pcDNA3.0) and tested for anti-EMT effects. The results obtained from Western blotting demonstrated a significant decrease in protein expression levels of HIF-1α and HIF-1 target genes upon fucoidan treatment. Furthermore, nuclear translocation and activity of HIF-1α were reduced. Fucoidan treatment significantly downregulated the expression levels of mesenchymal markers (N-cadherin and vimentin) but upregulated the expression levels of epithelial markers, zone obliterans-1, and E-cadherin. The overexpression of HIF1-α resulted in the protection of cells from fucoidan-mediated suppression of migration and invasion. The analysis of the collected data suggests that fucoidan could play a vital role in inhibiting EMT in human TNBC cells by downregulating the HIF1-α signaling pathway.
In conclusion, Fucoidan inhibited the activation and nuclear accumulation of HIF-1α. EMT regulators downstream of HIF-1α, including TWIST, Snail, CAIX, and GLUT-1, were also downregulated. Following this, there was a decrease in the expression levels of typical EMT markers, N-cadherin and vimentin, and an increase in the levels of ZO-1 and E-cadherin, ultimately leading to the inhibition of EMT and migration in TNBC cells under hypoxic conditions. Hence, the data suggests that fucoidan can potentially restrict EMT in human TNBC cells by suppressing the HIF1-α signaling pathway.
Source: Oncol Lett. 2019 Jul; 18 (1): 330–338. doi: 10.3892/ol.2019.10283
