Patients with chronic kidney disease (CKD) and impaired kidney function often develop mineral and bone disorders. These include metabolic imbalances in calcium, phosphorus, parathyroid hormone, vitamin D, and FGF23, resulting in abnormal bone structure and vascular calcification. Recently, CKD-mineral and bone disorder (CKD-MBD) has become one of the common complications occurring in CKD patients with stages G3a to G5D. Therefore, the development of new treatments for CKD-MBD is of great clinical importance.
Fucoidan, often abbreviated as FPS, is a sulfated carbohydrate abundant in fucose, a type of sugar, and is found in various marine organisms, including brown seaweeds and echinoderms, which are invertebrate marine animals. In recent years, it has been pointed out as a possible role as a therapeutic or adjuvant drug for CKD and osteoporosis. Studies by WHwang et al. and Jin et al. also found that low molecular weight FPS inhibits osteoclast differentiation and attenuates osteoporosis in vivo and in vitro. Therefore, it seems reasonable to assume that FPS targeting renal damage and bone abnormalities could be a new suitable therapeutic approach for CKD-MBD patients. However, crucial unanswered questions remain regarding FPS’s potential to improve renal damage and bone abnormalities, and the underlying in vivo and in vitro mechanisms.
In this blog, I would like to share the following study, “Fucoidan Ameliorates Renal Injury-Related Calcium-Phosphorus Metabolic Disorder and Bone Abnormality in the CKD–MBD Model Rats by Targeting FGF23-Klotho Signaling Axis” by Bu-Hui Liu et al. This study investigated the therapeutic effects of Fucoidan (FPS) from Laminaria japonica in rats with CKD-MBD, comparing it to calcitriol (CTR) and exploring its mechanisms in vivo and in vitro.
First, male rats were divided into four groups: Sham, CKD-MBD, FPS, and CTR. The CKD-MBD rat model was induced by adenine administration and unilateral nephrectomy, and the rats were administered either FPS or CTR or vehicle for 21 days after induction of renal injury. The study analyzed parameter changes related to kidney disease, including renal tubulointerstitial damage, calcium-phosphorus disorders, and bone lesions.
In the CKD-MBD model rats, significant changes in urinary Ca2+ and P4+, serum Ca2+, P4+, ALP, VD3, FGF23, and iPTH, and obvious decreases in TBBMD and FBBMD were observed compared to the sham-operated rats. Three weeks after inducing kidney damage in CKD-MBD model rats, HE staining revealed typical bone lesions, including resorption cavities in the cortical bone.
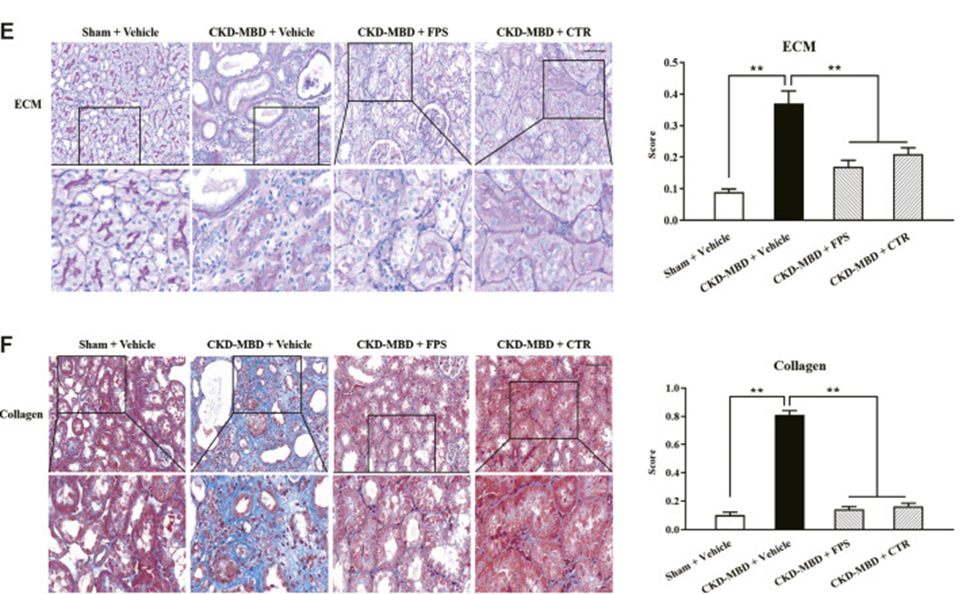
The researchers validated the influence of FPS and CTR on kidney injury in a rat model of CKD-MBD. As shown in Fig.1, observation under LM 3 weeks after induction of renal injury 1detected intact and transparent renal interstitium and open tubules in rats in the Sham group. In comparison, obvious renal tubulointerstitial injury, such as ECM accumulation and collagen deposition in the tubulointerstitial region of rats in the CKD-MBD group, was confirmed compared with rats in the Sham group. Three weeks of FPS or CTR treatment significantly improved ECM accumulation and collagen deposition in the rat tubulointerstitial region compared to the CKD-MBD group (See Fig. 1E, F).
The effects of FPS and CTR on urinary Ca2+ and P4+, serum Ca2+, P4+, VD3, FGF23, and BMD in CKD-MBD model rats were evaluated. Compared to control rats, rats with induced kidney injury showed higher urinary calcium, serum phosphorus, and FGF23 levels, along with lower urinary phosphorus, serum calcium, and vitamin D levels, and reduced bone mineral density in the femur and lumbar spine—all consistent with kidney dysfunction. After 3 weeks of FPS or CTR administration, CKD-MBD model rats showed significant improvements in urinary Ca2+, P4+, serum Ca2+, P4+, and VD3 levels, as well as serum FGF23 and BMD, compared with CKD-MBD rats.
This study investigated the impact of FPS and CTR on Klotho, FGF23, and FGFR1—key signaling molecules in the FGF23-Klotho axis—within the renal tubular interstitium and kidneys of CKD-MBD model rats, employing IHC staining and WB analysis. Following the induction of renal injury in CKD-MBD model rats, a notable decrease was observed in the immunohistochemical staining intensity of Klotho, FGFR1, and FGF23 within the renal tubular interstitium. Meanwhile, a significant decrease in the protein expression level of Klotho and an increase in the protein expression level of FGFR1 in the kidney were revealed compared with the Sham group rats. After administration of FPS or CTR for 3 weeks, the expression of Klotho in the renal tubular interstitium and kidney of CKD-MBD model rats was improved, respectively, compared with the CKD-MBD group rats. However, the expression of FGFR1 was not improved.
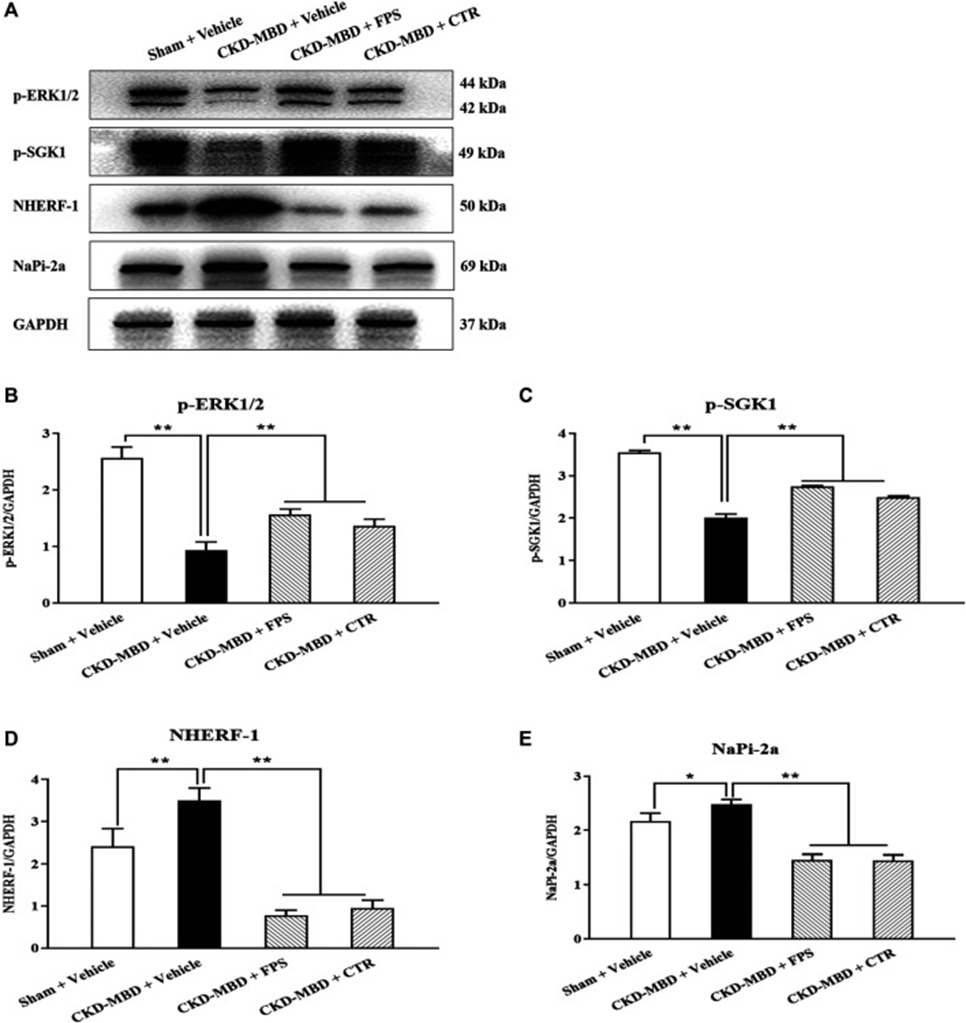
In CKD-MBD, the FGF23-Klotho pathway’s downstream ERK1/2-SGK1-NHERF-1-NaPi-2a pathway is crucial for phosphate reabsorption in proximal renal tubules. The effects of FPS and CTR on the protein expression levels of p-ERK1/2, p-SGK1, NHERF-1, and NaPi-2a in the kidneys of CKD-MBD model rats were observed by WB analysis. As shown in Figure 2A, after induction of renal injury, the kidneys of CKD-MBD model rats showed significantly decreased protein expression levels of p-ERK1/2 and p-SGK1 and increased protein expression levels of NHERF-1 and NaPi-2a compared with those of sham rats. After 3 weeks of FPS or CTR administration, the changes in the protein expression levels of p-ERK1/2, p-SGK1, NHERF-1, and NaPi-2a in the kidneys of CKD-MBD model rats were ameliorated compared with those of the CKD-MBD group rats ( Figures 2B–E ).
The result showed that the study demonstrated that FPS, a natural anti-renal dysfunction drug similar to CTR, improves renal injury-associated calcium-phosphorus metabolic disorders and bone abnormalities in CKD-MBD model rats. This study revealed a correlation between the beneficial effects of FPS on phosphorus resorption (in vivo and in vitro) and the regulation of the FGF23-Klotho and ERK1/2-SGK1-NHERF-1-NaPi-2a pathways within the kidney. This study offers pharmacological proof that FPS is a direct contributor to CKD-MBD treatment.
Source: Front Pharmacol. 2021 Jan 28;11:586725. doi: 10.3389/fphar.2020.586725
