Intestinal epithelial cells play a crucial role in allowing food to enter the body while also acting as a strong defense against harmful compounds like food and bacterial toxins. However, their barrier function can be compromised when they come into contact with dAGEs, primarily found in food.
In this blog, I would like to share the study, “High Molecular Weight Fucoidan Restores Intestinal Integrity by Regulating Inflammation and Tight Junction Loss Induced by Methylglyoxal-Derived Hydroimidazolone-1” by Jae-Min Lim et al. The research examined how wakame-derived high molecular weight fucoidan (HMWF) protects the gut from damage caused by methylglyoxal-derived hydro imidazoline-1 (MG-H1), a type of dietary advanced glycation end product (dAGE). The study used human colon cancer cell line (Caco-2) cells and ICR mice.
First, to investigate the cytotoxicity of HMWF in human colon cancer cell line (Caco-2) cells, 3-[4,5-dimethylthiazol-2-yl]-2,5-diphenyltetrazolium bromide (MTT) assay was performed with various concentrations of HMWF. Caco-2 cells were treated with HMWF for 24 hours. In comparison to the control group, the cell viability showed a significant decrease of 90% at a concentration of 500 μg/mL and 80% at a concentration of 1000 μg/mL (as shown in Figure 1). The highest absorption rate of fucoidan in Caco-2 cells was observed at a concentration of 500 μg/mL.
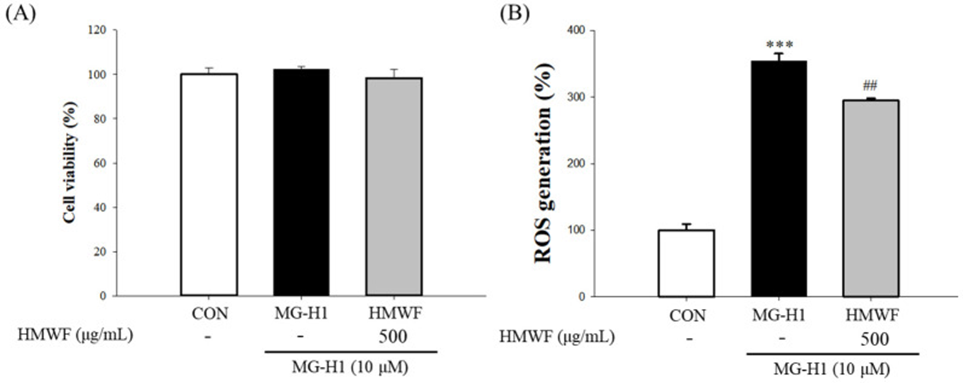
The highest absorption rate of fucoidan in Caco-2 cells was observed at a concentration of 500 μg/mL. The highest absorption rate of fucoidan in Caco-2 cells was observed at a concentration of 500 μg/mL. To gain a better understanding of how HMWF safeguards cells from the harmful effects of MG-H1-induced cell stress, we embarked on an in-depth investigation. In this study, we exposed Caco-2 cells to both MG-H1 and HMWF concurrently, and carefully examined cell viability and ROS generation. Strikingly, our findings indicated that there were no significant reductions in cell viability observed in the control group, MG-H1 group, or the MG-H1 + HMWF group (as illustrated in Figure 1B).
The simultaneous treatment of Caco-2 cells with MG-H1 and HMWF allowed for the assessment of cell viability and ROS generation, providing further insight into the protective effects of HMWF against MG-H1-induced cellular stress. The results obtained from this study are depicted in the Figure 1A.
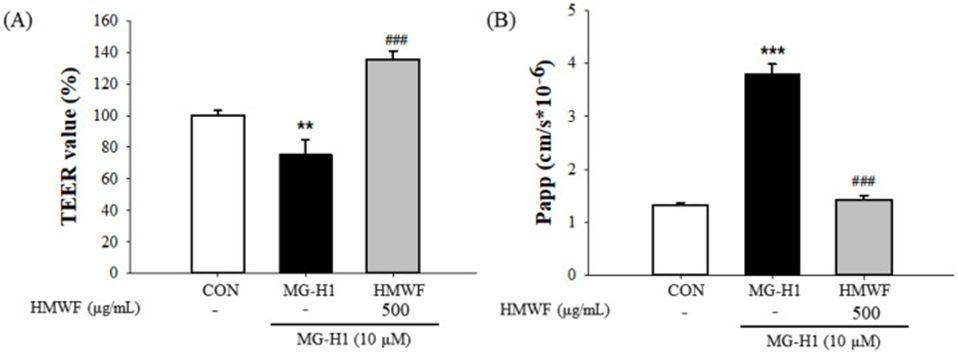
To evaluate the protective effect of HMWF against intestinal barrier dysfunction caused by MG-H1 treatment in differentiated Caco-2 cell monolayers, transepithelial electrical resistance (TEER) was measured. The TEER values of the cells treated with MG-H1 showed a significant decrease compared to the untreated control cells, indicating a notable decrease in the integrity of the Caco-2 monolayer. However, TEER values after HMWF + MG-H1 treatment were significantly increased compared to MG-H1 treatment, protecting the monolayer integrity in Caco-2 cells, as seen in Figure 2A. Furthermore, in control, MG-H1, and MG-H1 + HMWF treatments, the permeability coefficient (Papp) was significantly increased in MG-H1-treated cells compared to control cells and significantly decreased in MG-H1 + HMWF-treated cells compared to MG-H1-treated cells as shown in Figure 2B.
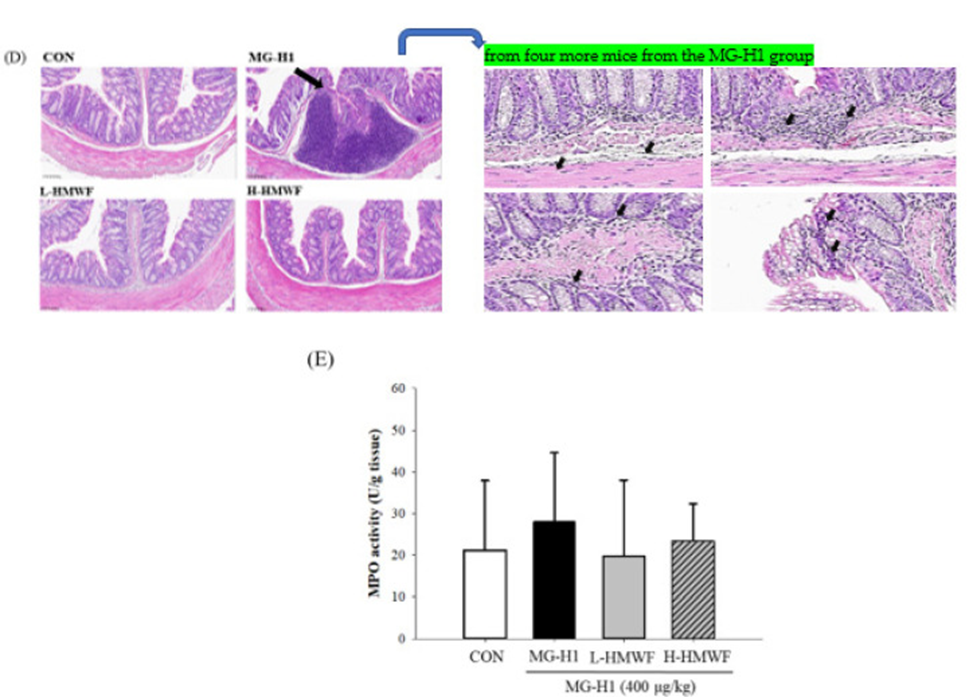
Next, to examine whether HMWF administration reduces colonic injury in mice treated with MG-H1, hematoxylin, and eosin staining was performed to evaluate histopathological changes in colonic tissues after oral administration of FITC-dextran. No epithelial damage or inflammatory cell infiltration was observed in the control group (Figure 3D). In the MG-H1 + HMWF treatment group, lymphoid aggregates could be effectively reduced, and MG-H1 injection increased myeloperoxidase (MPO) activity. HMWF treatment reduced MG-H1-induced MPO activity (Figure 3E). Thus, HMWF treatment could suppress MPO-mediated oxidative stress and colonic inflammation induced by MG-H1.
The integrity of the intestines is thought to be influenced by the expression of TJ proteins. To demonstrate the protective effect of HMWF against TJ damage induced by MG-H1 treatment, we measured the mRNA and protein expression levels of TJ markers, such as ZO-1, occludin, and claudin-1. The observations indicate TJ marker expression at the mRNA and protein levels in mouse colon tissues determined whether HMWF administration inhibited MG-H1-induced TJ disruption, and the results suggest that HMWF treatment may restore intestinal barrier dysfunction by restoring TJ loss caused by MG-H1 treatment.
The study aimed to determine if treating Caco-2 cells and mice with MG-H1 would result in increased expression of RAGE mRNA and protein. This is important because the binding of AGE to RAGE can trigger cell signaling pathways and cause intestinal inflammation and disease. In Caco-2 cells exposed to MG-H1, RAGE expression was significantly increased at both the mRNA and protein levels. At the same time, the administration of HMWF treatment effectively countered the elevation of RAGE expression, both in mRNA and protein levels, triggered by MG-H1 treatment. The results suggest that HMWF treatment may play an important role in mediating MG-H1-induced RAGE expression.
HMWF treatment prevented MG-H1-induced expression of tight junction markers including zonula occludens-1, occludin, and claudin-1 at the mRNA and protein levels in Caco-2 cells and mouse colonic tissues. Also, in Caco-2 and MG-H1-treated mice, HMWF plays an important role in preventing receptor for AGEs (RAGE)-mediated intestinal damage. Based on these results, it can be inferred that HMWF may be instrumental in preventing the dysfunction of the intestinal barrier caused by AGE.
Source: Mar Drugs. 2022 Sep; 20(9): 580. doi: 10.3390/md20090580
