Ulcerative colitis and Crohn’s disease are among the conditions categorized as inflammatory bowel disease (IBD), which refers to chronic inflammation in the intestines. IBD not only causes gastrointestinal symptoms such as diarrhea and abdominal pain but also affects the entire body, causing stomatitis, joint pain, skin disorders, and more. When considering the long-term outlook, it is important to note that this condition is characterized by a pattern of alternating phases, where symptoms worsen during relapse and subside during periods of calm known as remission. In recent years, the number of patients has been rapidly increasing, especially in developed countries, but the cause of IBD is unknown, and as no treatment can completely cure it, it has been designated as an intractable disease by the government.
So, in this blog, I would like to share the study, “Fucoidan enhances intestinal barrier function by upregulating the expression of claudin-1” by Atsushi Iraha et al. In their research, the scientists investigated the ability of fucoidan to safeguard human intestinal epithelial cells against oxidative stress-induced barrier disruption.
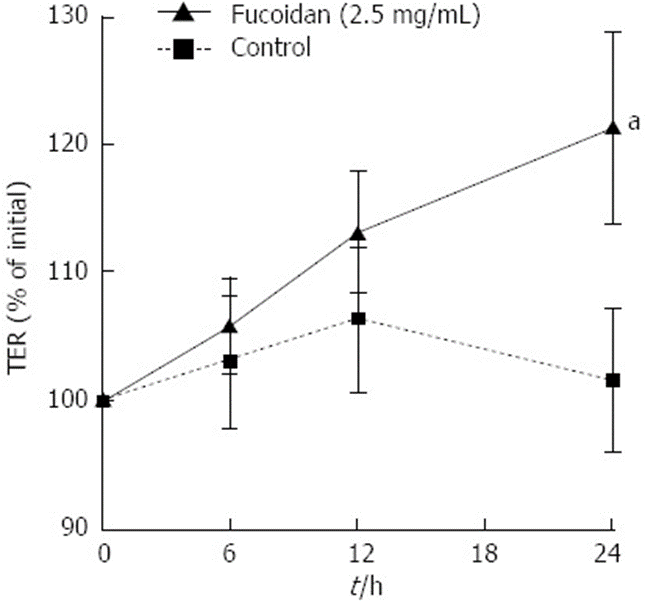
The Caco-2 cell monolayer model demonstrates that H2O2 is the mediator of barrier function disruption due to oxidative stress. Therefore, the integrity of polarized Caco-2 cell monolayers is determined by measuring the transepithelial resistance (TER). First, the researchers examined the effect of fucoidan on the protective function of Caco-2 monolayers. In order to understand the relationship between fucoidan and epithelial resistance, we conducted experiments on fully polarized Caco-2 cell monolayers. By doing so, we aimed to determine whether fucoidan directly increases resistance or if it achieves this by promoting epithelial cell proliferation and upregulating TER. Fully polarized Caco-2 cell monolayers exhibited a TER of approximately 600 Ωcm2. Due to the inability of polarized Caco-2 cells to undergo further proliferation, the researchers could investigate the specific impact of fucoidan on the function of the intestinal epithelial barrier. According to Figure 1, the use of Fucoidan resulted in a significant increase in TER when compared to the control group. This increase suggests an improvement in the function of the intestinal epithelial barrier.
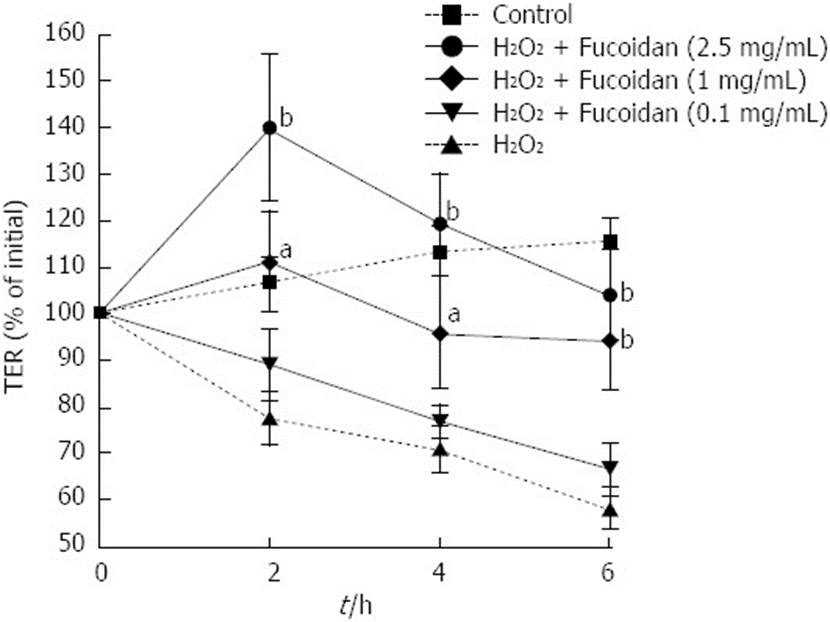
Next, the study focused on the preventive effect of fucoidan on epithelial cell damage. To evaluate the effect of fucoidan on intestinal epithelial barrier function, fully polarized Caco-2 cell monolayers were damaged by H2O2. H2O2 was added to the lower well of the Transwell®, and changes in intestinal epithelial barrier function were monitored by measuring TER. As shown in Figure 2, H2O2 disrupted the epithelial barrier function in a time-dependent manner. In contrast, treatment with fucoidan prevented H2O2-induced intestinal epithelial damage at early time points. At both concentrations of 1 and 2.5 mg/mL, high doses of fucoidan exhibited the ability to prevent the destruction of the epithelial barrier, even during the latter stages. Thus, fucoidan prevented H2O2-induced intestinal epithelial barrier destruction in a dose-dependent manner.
They examined whether H2O2 increases the intercellular permeability of Caco-2 cell monolayers after epithelial injury and whether fucoidan can prevent this effect. In this experiment, we performed an FD4 flux assay. H2O2 significantly increased FD4 flux to the lower well. The administration of fucoidan 30 minutes prior to the introduction of H2O2 resulted in a significant inhibition of the increase in FD4 flux across the Caco-2 cell monolayer to the lower well. Based on the results, it can be concluded that H2O2 negatively affected the functionality of the Caco-2 cell monolayer, but the presence of fucoidan prevented the disruption of the intestinal epithelial barrier function.
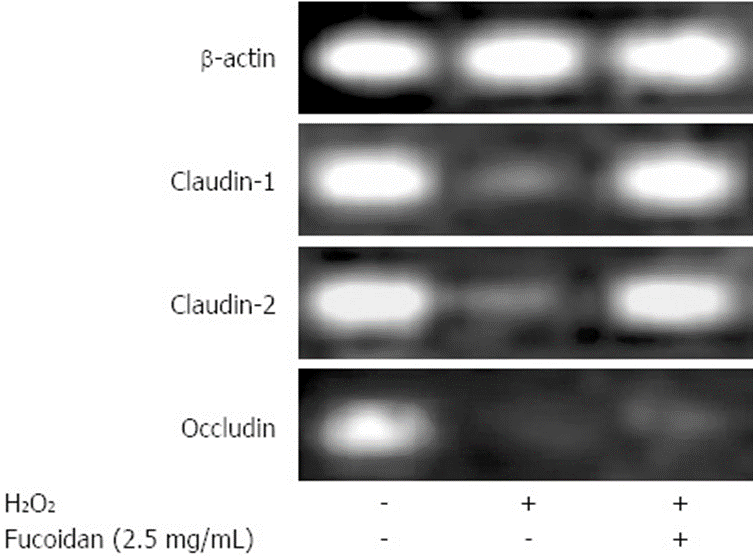
An analysis was carried out to investigate how fucoidan treatment enhances the function of the intestinal epithelial barrier, specifically by examining the impact of fucoidan on the mRNA expression of key tight junction (TJ)-associated proteins. As shown in Figure 3, Caco-2 cells endogenously expressed claudin-1 and claudin-2, and occludin. H2O2 reduced the mRNA expression of these proteins. Furthermore, pretreatment with fucoidan mitigated the decrease in claudin-1 and claudin-2 mRNA expression, but not that of occludin mRNA. These results suggest that fucoidan treatment strongly induced the expression of claudin-1 and claudin-2, which promote intestinal epithelial barrier function, and that fucoidan promoted intestinal epithelial barrier function via the direct upregulation of tight junction proteins in IECs.
In addition, the researchers utilized immunofluorescence microscopy to analyze the influence of fucoidan on the intracellular positioning of claudin-1. In control cells, claudin-1 expression was found to be intact and at high levels on the cell surface. H2O2 strongly disrupted the integrity of claudin-1 and reduced its expression. Fucoidan significantly reduced the damage caused by H2O2, leading to cell integrity restoration and increased claudin-1 expression. This suggests that fucoidan effectively protected claudin-1, a tight junction protein, from H2O2-induced destruction.
The results show that fucoidan can directly increase the expression of multiple TJ proteins, thus enhancing the function of the epithelial barrier. Fucoidan’s ability to improve the protective function of epithelial cells and promote their regeneration suggests that it could be a viable treatment for IBD.
Source: World J Gastroenterol. 2013 Sep 7; 19(33): 5500–5507. doi: 10.3748/wjg.v19.i33.5500

Hi, my name is Rafsan. I need your help. My uncle in Palestin Gaza need help. They don’t have food. Please help me. I need 1000$ to help my family. My WhatsApp number is +8801601701933.
I have known the situation in Gaza in Palestine, however, I do not donate to individuals, also I do not have such money. I contribute a small amount by going through UNICEF to help all equally.
I am very sorry for your uncle’s situation, but all of Gaza’s people are suffering, not only your uncle’s family.
When Trump is won in the coming US election, every war will be finished.
People in the world pray for finishing every war.