Sepsis is a life-threatening response or condition in which bacteria are causing some infectious disease that proliferates and inflammation spreads throughout the body, resulting in severe organ damage and seriousness. Quite often, an infectious disease triggers Sepsis.
Any infectious disease can trigger Sepsis, especially in infants who are not immune, the elderly, people with chronic illnesses such as diabetes, underlying conditions, cancer, and undergoing similar treatment. Especially people with weakened immunity are at increased risk of developing Sepsis from an infection.
Examples of causative bacterium include streptococcus, staphylococcus, Escherichia coli, and Pseudomonas aeruginosa. The bacterial infection causes various infectious diseases such as respiratory tract infections, skin suppuration, pneumonia, liver, kidney, and intestine infections.
In addition to bacteria, infectious diseases can also be caused by viruses such as influenza virus, fungi, mold, and parasites.

Also, in a state of “neutropenia,” in which neutrophils, a type of white blood cell, decrease, the patient becomes more susceptible to infections and is more likely to develop Sepsis. Neutropenia can be hereditary, congenital, or acquired. It is also common in cancer patients receiving chemotherapy with anticancer drugs.
Fucoidan is a sulfated polysaccharide derived from brown algae reported to perform multiple biological activities, including immunostimulation. For example, Fucoidan regulates the function of various immune cells such as lymphocytes, dendritic cells (DCs), natural killer (NK) cells, and neutrophils.
So, in this blog, I want to share the study “Fucoidan Enhances the Survival and Sustains the Number of Splenic Dendritic Cells in Mouse Endotoxemia” by Eun-Ju Ko et al. The study investigated Fucoidan and its beneficial effects on endotoxemia induced by LPS (bacterial lipopolysaccharide), a septic model in mice. The focus of the study was on survival rates and the spleen function of the mice upon treatment.
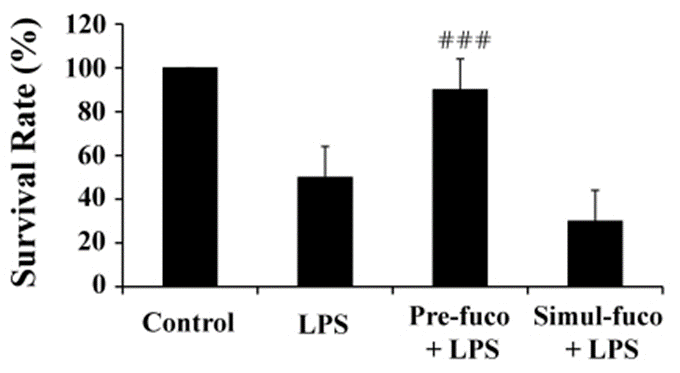
First, to investigate whether Fucoidan may positively affect the survival of mice with endotoxemia, they injected 30 mg/kg LPS, a lethal dose, along with 100 mg/kg fucoidan. They then evaluated the mortality of the mice over the next five days. As a result, LPS significantly decreased the survival rate. Interestingly, pretreatment with Fucoidan significantly reduced LPS-induced mortality (Fig. 1).
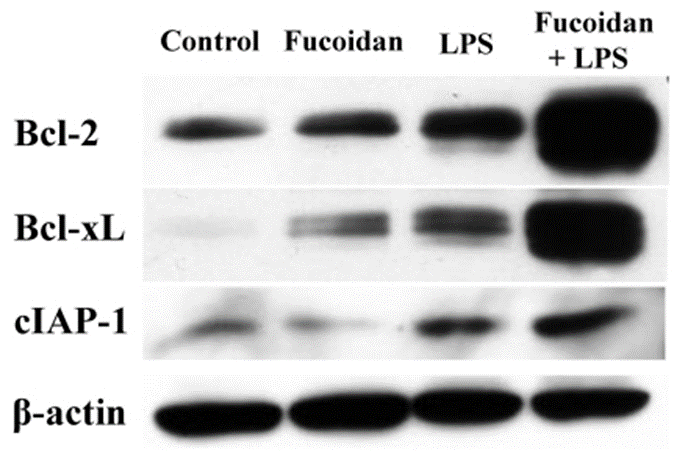
According to Western blot analysis, the spleen cells of LPS/fucoidan-treated mice showed a higher expression of anti-apoptotic molecules compared to those of LPS-treated mice. Furthermore, fucoidan-treated spleen cells were more responsive to mitogens. It indicates that Fucoidan and LPS have a synergistic effect on the expression of anti-apoptotic molecules in mouse spleen cells, suggesting that these two therapies may enhance the viability of spleen cells against apoptotic signals.
These results demonstrate that fucoidan pretreatment has a beneficial impact on the survival rate and function of the spleen in mice with endotoxemia (Fig. 2).
The protective effect of Fucoidan on antigen-specific and memory immune responses in endotoxin hosts is the ability to protect DC and spleen cells from endotoxemia, which can expand to use both clinically and in future endotoxin studies. However, the detailed mechanisms by which fucoidan acts need to be further investigated.