In this blog, I am going to share about Proliferative Vitreoretinopathy (PVR) and the Fucoidan effect. While undergoing PVR treatment, and that also includes surgery in most cases, there are factors that induce proliferative tissue to appear after surgery. Due to this reason, multiple surgeries may be required. The crystalline lens will be removed if peripheral treatment is required after surgery, even if the crystalline lens is left in the first surgery. However, even after several surgeries, the sight may be lost.
Proliferative Vitreoretinopathy (PVR) is a condition that causes severe blinding complications of rhegmatogenous retinal detachment from the aging phenomenon in a broad sense.
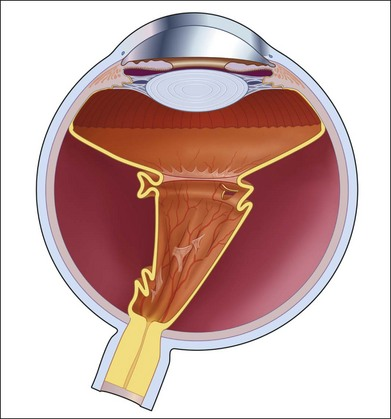
This tissue resembles the white of a raw egg. It is called the “glass body” between the retina (fundus), and it gets inflamed to become “liquefies.” after that, the lens in the eye causes a retinal detachment. Then the neural retina is detached from the retinal pigment epithelial cells. When it becomes “liquefies,” which move in the eyeball, pulling the retina and forming either “cruck” in a part of the retina or a part of the retina atrophy and “circular hole.” When a small “hole” is created, water enters under the retina through the fissure or circular hole, and the retina peels off. Apart from that, it is also a condition that occurs when diabetic retinopathy, in which blood vessels in the retina are abnormal due to blood sugar, worsens. Also, it is stated that the results of surgery are lower than those of typical retinal detachment.
Epithelial-mesenchymal transition (EMT) of retinal pigment epithelial (RPE) cells are thought to play a pivotal role in the pathogenesis of PVR. EMT is the biological mechanism that the healing of retinal detachment and surgical lacerations, which temporarily loses the properties of the mature epithelial system and induces conversion to mesenchymal stem cells with high proliferative and regenerative capacity. Still, the proliferative response occurs in situations where inflammation persists. If it is repeated chronically, it causes abnormalities and causes fibrosis in the eye. Therefore, suppressing EMT in RPE cells is an effective way to prevent PVR. On the other hand, fucoidan, a sulfated polysaccharide contained in brown algae, is studied and proven to have a preventive and improving effect of kidney interstitial fibrosis and diabetic nephropathy by suppressing EMT. Hence, the study,” Protective Effects of Fucoidan on Epithelial-Mesenchymal Transition of Retinal Pigment Epithelial Cells and Progression o Proliferative Vitreoretinopathy,” by Yao Zhang et al., has studied the effect of fucoidan on RPE cells’ EMT and PVR progression.
First, as a result of adding fucoidan derived from Hibamata to RPE cells and observing the state of the cells 48 hours later, it was shown that there was no effect on the cell viability and the toxicity to RPE cells was extremely low (Fig. 1).
Next, researchers investigated the effect of fucoidan on EMT. RPE cells were cultured in the presence of the EMT inducer TGF-β1, and the expression status of the epithelial marker E-cadherin, the mesenchymal marker smooth muscle α-actin (α-SMA), and fibronectin were used as an index. As a result, in the non-addition group, a decrease in E-cadherin and an increase in mesenchymal markers were observed in the presence of TGF-β1and EMT was induced. Additionally, they found that in the fucoidan-added group, the growth and decrease of each marker associated with TGF-β1 treatment was alleviated, and the appearance of EMT was not exhibited. (Fig. 2). This result indicates that fucoidan acted to suppress EMT in RPE cells.
Finally, an animal study inducing PVR in the rabbit’s right eye examined whether fucoidan had the actual effect of stopping PVR progression. A group is prepared, in which fucoidan is injected into the vitreous body, and a target group in which phosphoric acid slow hygiene treatment water (PBS) is injected. This is followed by observing the retina’s appearance by a non-invasive imaging method called optical coherence tomography (OCT). As a result of investigating the progress of PVR, the target who received PBS developed extensive retinal detachment and retinal foramen, as seen in the arrow in the figure. In contrast, the group treated with fucoidan had a slight focal contraction and a moderate vascular serpentine (Fig. 3). These results indicate that fucoidan suppresses EMT in RPE cells and has an inhibitory effect on PVR progression. The above suggests that fucoidan may be used for PVR treatment. It is expected that fucoidan will also be used in the ophthalmic field in the future.

Fig. 1) Effect of fucoidan on PRE cell viability
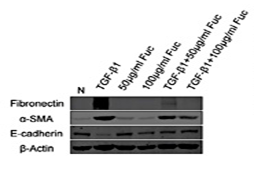
Fig.2) Inhibitory effect of fucoidan on TGF-β1-induced EMT
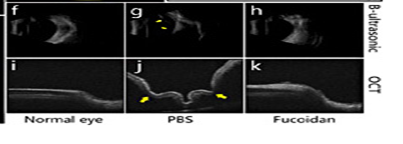
Fig. 3) ) Fucoidan’s PVR progression suppression effect in the rabbit model