Patients recovering from acute SARS-CoV-2 infection are likely to develop long-term sequelae, which include lung injury, inflammation, neurodegeneration, etc. These conditions are caused by mitochondrial dysfunction. Therefore, searching for alternative therapies is essential to reintegrate cellular homeostasis in SARS-CoV-2-infected individuals.
Fucoidan is a polysaccharide derived from seaweed, and as shared in previous studies, it is proven to have anti-inflammatory, antiviral, and immune-enhancing properties. Additionally, fucoidan inhibits SARS-CoV-2 infection in Vero E6 cells (monkey kidney epithelial cells) via a sulfated polysaccharide tightly binding to the SARS-CoV-2 S protein, preventing viral internalization in vitro. Based on these bioactivities, fucoidan may be used as an alternative treatment along with prescribed medical therapy for COVID-19 recovery. Therefore, in this blog, I would like to familiarize you with the study “Effect of Fucoidan on the Mitochondrial Membrane Potential (ΔΨm) of Leukocytes from Patients with Active COVID-19 and Subjects That Recovered from SARS-CoV-2 Infection” by Karina Janice Guadalupe Díaz-Resendiz et al.
The above study investigated the effects of fucoidan (20 μg/mL) treatment on mitochondrial membrane potential (using ΔΨm, a cationic cyanine dye, 3,3′-dihexyloxacarbocyanine iodide (DiOC6(3)) in human peripheral blood. Aimed to determine the ex-vivo effects of mononuclear cells (HPBMC) isolated from healthy control (HC) subjects, COVID-19 patients (C-19), and subjects recently recovered from COVID-19 was investigated. First, treatment with fucoidan (20 and 50 μg/mL) improved carbonyl cyanide 3-chlorophenylhydrazone (CCCP, 150 μM ) induced ΔΨm loss.
The phase 1 data showed that the C19 and R1 groups show up to 96% loss of ΔΨm relative to the HC group. The group had active COVID-19 and those who had recently recovered from an infection, respectively. (See Figure 1). However, fucoidan treatment (20 μg/mL) induces a significant recovery of ΔΨm (70%) in subjects in the R1 group (basal R1 vs. R1 with fucoidan). In contrast, in C-19 patients, fucoidan treatment did not significantly restore ΔΨm (basal C-19 vs. C-19 containing fucoidan). (See Figure 1)
Phase 1 results show that treatment with 20 μg/mL fucoidan restores ΔΨm in subjects who recovered 40 ± 13 days after infection with COVID-19.
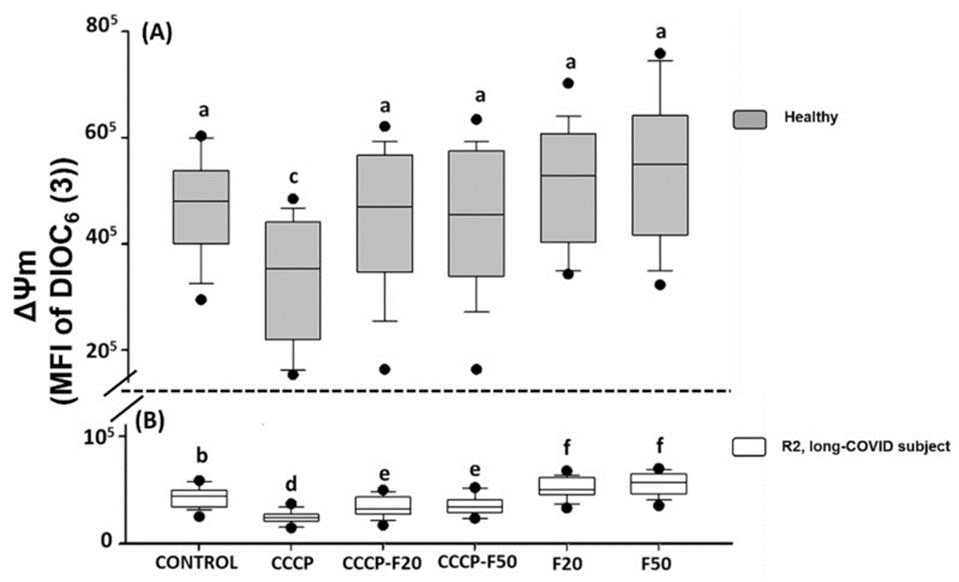
Phase 2 data showed that thirty-eight subjects (16 males, 22 females) with a mean age of 41 years (range = 21–74 years) participated in the study. The healthy group consisted of 8 males and 11 females with a mean age of 41 (range = 21–69) years. The subjects (R2, n = 19) who recovered 11 months after COVID-19 had a mean age of 41 (range = 24–74) years, of whom eight were male and 11 were female.
The results show that treatment with fucoidan induces restoration of ΔΨm in HPBMCs in different experimental groups, CCCP + F50, F20, and F50 in H subjects (See Figure 2A) and R2 subjects CCCP + F20, CCCP + F50, F20 (See Figure 2B) and it induced recovery of F50. On the other hand, figure 3 shows that ΔΨm is significantly reduced in R2 versus healthy subjects. Yet, when these cells were treated with fucoidan 20 and 50 μg/mL, HPBMCs were substantially lower than R2 controls. It significantly improved the leverage parameter but did not restore ΔΨm relative to healthy controls. Phase 2 results showed that treatment with 20 and 50 μg/mL fucoidan restored her ΔΨm in the recovered subject 11 months after COVID-19. In conclusion, the overall result was that fucoidan significantly restored ΔΨm in HPBMCs, suggesting that fucoidan treatment may help improve mitochondrial homeostasis after SARS-CoV-2 infection. Hence, fucoidan may be included as a potential therapeutic to prevent long-term sequelae of COVID-19, and mitochondria are therapeutic targets to restore cellular
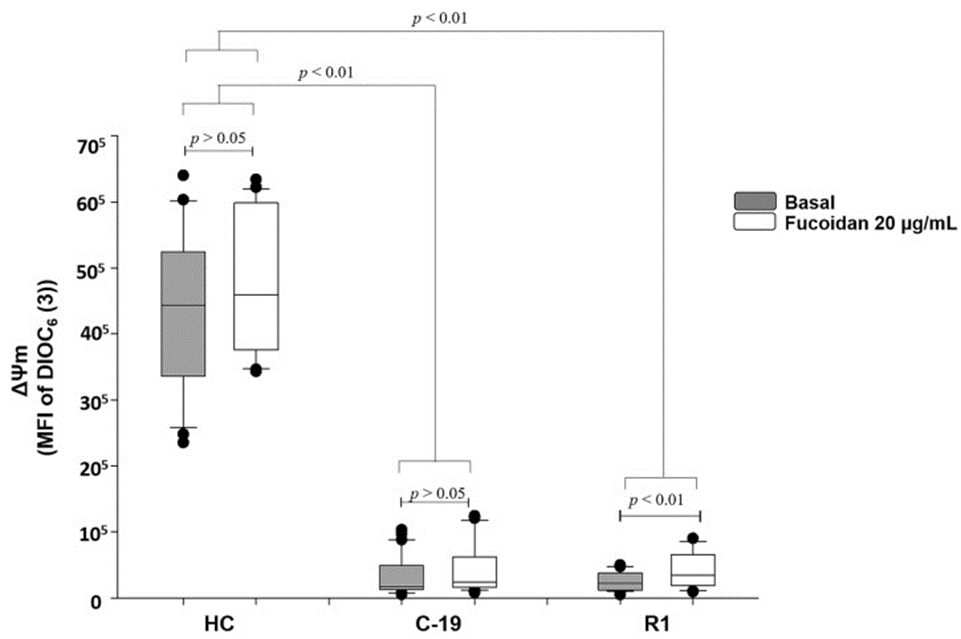
Fig.- 1) Ex-Vivo Fucoidan Treatment in HPBMCs of HC, C-19, and R1 Subjects
Source: Mar Drugs. 2022 Feb; 20(2): 99. doi: 10.3390/md20020099