CKD, or Chronic Kidney Disease, is a gradual failure of the kidney’s function over time. Unfortunately, in patients with chronic kidney disease, there is a high risk of bone fracture with a decline in renal function and onset of bone structural abnormalities.
In addition, when fractures restrict physical activity, they weaken muscles further. Hence, appropriate management of chronic kidney disease-mineral and bone disorder (CKD-MBD) is necessary to break this vicious cycle that leads to bedriddenness and death. Therefore, developing a new treatment for CKD–MBD is also essential in the clinic.
On the positive side, Fucoidan (FPS), a natural compound of Laminaria japonica, has often been used to ameliorate renal dysfunction in CKD. However, it is not yet confirmed if FPS can improve CKD-MBD.
Thus, in this blog, I would like to share with you the study “Fucoidan Ameliorates Renal Injury-Related Calcium-Phosphorus Metabolic Disorder and Bone Abnormality in the CKD–MBD Model Rats by Targeting FGF23-Klotho Signaling Axis” by Bu-Hui Liu et al.
The previous study reported that the FGF23-Klotho signaling axis helps in regulating mineral and bone metabolism disorders in CKD-MBD. So, this study further clarifies the therapeutic effects of FPS in CKD-MBD model rats and its underlying mechanisms in vivo and in vitro compared to calcitriol (CTR).
First, 28 rats were randomly divided into four groups, seven rats in the sham-operated group (the Sham group), seven rats in the CKD–MBD model group (the CKD–MBD group), seven rats in the FPS-treated group (the FPS group) and seven rats in the CTR-treated group (the CTR group) randomly.
CKD-MBD rat models were induced by adenine administration and single nephrectomy. They received either FPS or CTR or vehicle after induction of renal injury for 21 days. Changes in parameters associated with renal dysfunction and renal tubulointerstitial injury, calcium-phosphorus metabolism disorders, and bone lesions were analyzed, respectively.
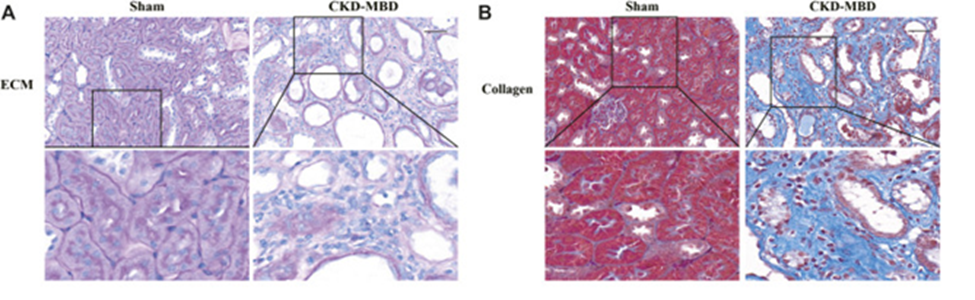
PAS and Masson staining showed that continuous adenine administration to rats at a safe and effective dose of 150 mg/kg/day resulted in tubular atrophy, interstitial cell infiltration, ECM (excessive extracellular matrix) accumulation, and collagen deposition in the tubulointerstitial area. In addition, it has been shown to cause significant renal tubulointerstitial damage three weeks after induction of renal injury. (Figure 1A, B)
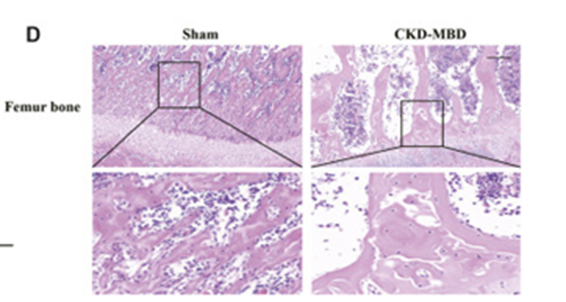
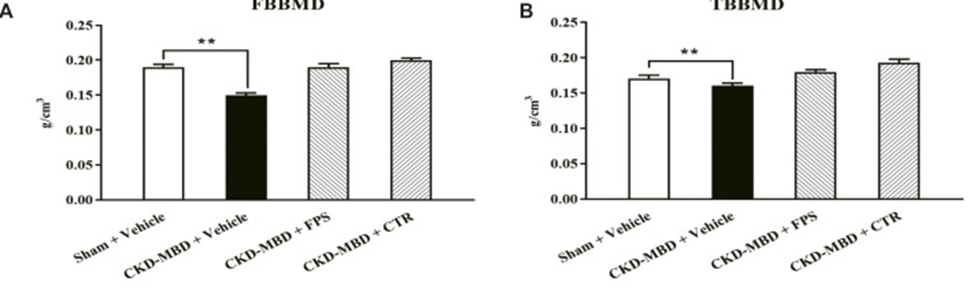
Next, they examined indices of urinary Ca2+ and P4+, serum Ca2+, P4+, ALP, VD3, FGF23 and iPTH, and TBBMD, FBBMD, and femoral pathological lesions in sham-operated rats and CKD-MBD models. As indicated by HE staining, CKD-MBD model rats three weeks after induction of renal injury revealed typical bone lesions with resorptive cavities in cortical bone. (Fig. 1D)
After three weeks of treatment with FPS or CTR, apparent renal tubulointerstitial damage, such as ECM accumulation and collagen deposition in the tubulointerstitial area of CKD-MBD group rats, was observed in the tubulointerstitial area of FPS and CTR group rats. Also, ECM accumulation and collagen deposition in the region were significantly improved compared to rats in the CKD-MBD group.
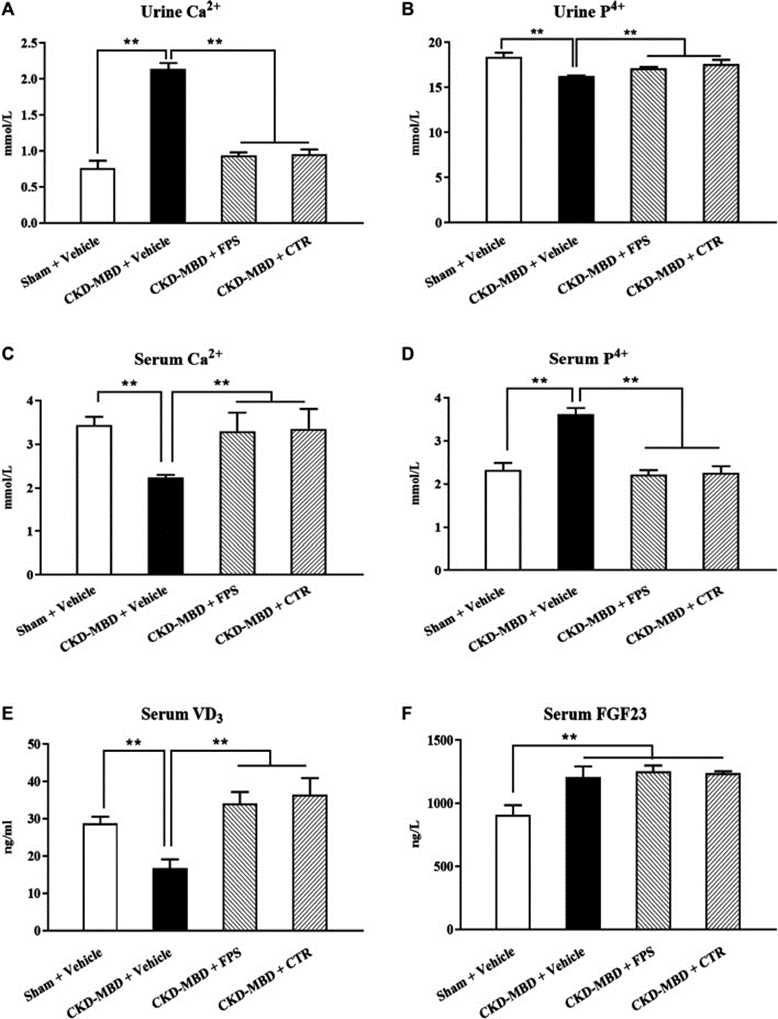
They evaluated the effects of FPS and CTR on levels of urinary Ca2+ and P4+, serum Ca2+, P4+, VD3 and FGF23, and BMD in CKD-MBD model rats. After three weeks of treatment of FPS or CTR, serum FGF23 and BMD, urinary Ca2+, P4+, serum Ca2+, P4+, and VD3 in CKD-MBD model rats were significantly improved compared with CKD after CKD. (Figure 2A–E and Figure 3A, B)
The ERK1/2-SGK1-NHERF-1-NaPi-2a pathway, downstream of the FGF23-Klotho signaling axis, plays an essential role in phosphate reabsorption in proximal tubular epithelial cells in CKD-MBD. By WB analysis, we observed the effects of FPS and CTR on the protein expression levels of p-ERK1/2, p-SGK1, NHERF-1, and NaPi-2a in the kidney of CKD-MBD model rats. As shown in Figure 7A, after induction of renal injury, the protein expression levels of p-ERK1/2 and p-SGK1 were downregulated. Also, the protein expression levels of NHERF-1 and NaPi-2a were upregulated in the kidney.
In conclusion, these results showed pharmacological evidence that FPS directly contributes to treating CKD-MBD.
Source: Front Pharmacol. 2020; 11: 586725 DOI: 10.3389/fphar.2020.586725