Inflammatory bowel disease (IBD), encompassing Crohn’s disease (CD) and ulcerative colitis (UC), is a complex, chronic, and multifactorial gastrointestinal disease of unknown origin that is characterized by periods of intestinal inflammation that relapse and remit.
Fucoidan, a sulfated polysaccharide derived from brown algae, in contrast, is a recognized anti-inflammatory agent; furthermore, research indicates that fucoidan extracts might also help regulate oxidative stress.
In this blog, I would like to share the following study, “Oral Macrocystis pyrifera Fucoidan Administration Exhibits Anti-Inflammatory and Antioxidant Properties and Improves DSS-Induced Colitis in C57BL/6J Mice” by Tauseef Ahmad et al. The research reports significant antioxidant and anti-inflammatory properties of fucoidan extracts from Macrocystis pyrifera which is called Giant Kelp (MPF and DP-MPF) in a model of acute colitis.
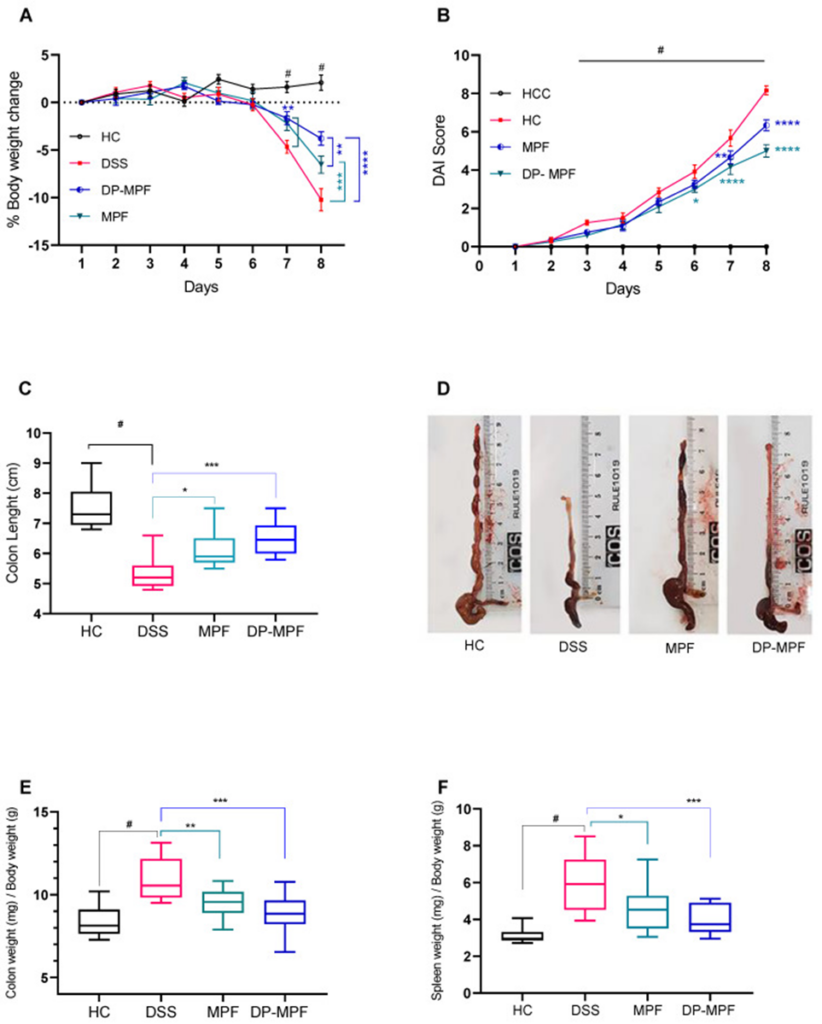
The impact of fucoidan extract, MPF, and DP-MPF was investigated in an acute colitis mouse model induced by dextran sulfate sodium (DSS). Oral administration of DSS reproduces human ulcerative colitis symptoms in mice, such as weight loss, blood in the stool, diarrhea, and colon shortening. First, C57BL/6J male mice were administered 3% DSS for 7 days, and MPF and DP-MPF were orally administered at a dose of 400 mg/kg body weight. As shown in Figure 1, MPF and DP-MPF significantly prevented weight loss, improved the DAI, restored colon length, decreased wet colon weight and splenomegaly, and enhanced overall histopathological scores.
Hematoxylin and eosin (H&E) stained tissue sections were used to evaluate the histopathology of the proximal colon (PC) and distal colon (DC). H&E stained sections from mice in the HC group showed no signs of inflammation or damage to the colonic mucosal architecture in the stained sections. DSS-treated mice exhibited significant colonic crypt damage, epithelial disruption, goblet cell depletion, submucosal edema, and mucosal inflammatory cell infiltration, predominantly in the distal colon. This resulted in higher cumulative histology scores in the DC and PC in the DSS-treated group. In contrast, MPF and DP-MPF treatment offered significant protection against colonic inflammation in mice, preserving the colon’s structure, reducing goblet cell loss, and limiting inflammatory cell infiltration.
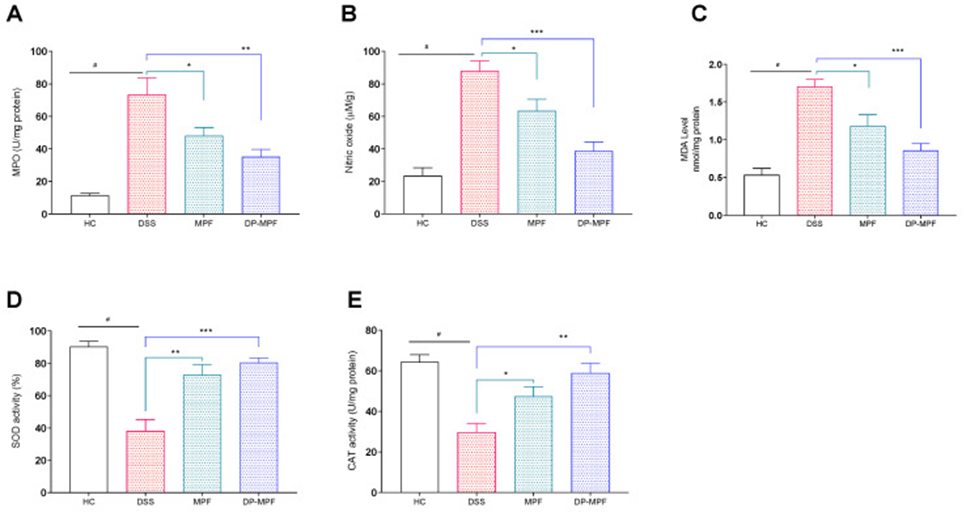
MPF and DP-MPF reduced oxidative stress markers MPO, NO, and MDA. The protective role of MPF and DP-MPF in oxidative stress conditions was evaluated by assessing the levels of oxidative stress markers, such as MPO, NO, and MDA, in DCs. The application of DSS treatment resulted in a significant and observable elevation in the levels of these specific markers, as clearly illustrated in Figures 2A–C. Figures 2A–C illustrate that the MPF and DP-MPF treatments resulted in significantly lower levels compared to the DSS group, with each treatment showing a distinct level of reduction.
MPF and DP-MPF increased the levels of antioxidant enzymes SOD and CAT. Antioxidant enzymes such as SOD and CAT are essential in protecting tissues from oxidative stress. DSS treatment significantly reduced the activity of SOD enzyme in DCs by 38.10% compared with healthy mice (HC) (See Figure. 2D, E). In contrast, MPF and DP-MPF treatment significantly increased the activity of SOD compared with the DSS group (See Figure. 2D). Consistent with SOD activity, DSS treatment significantly decreased CAT activity in DCs compared with healthy controls (HCs). However, MPF and DP-MPF treatment significantly restored CAT activity compared with the DSS group (See Figure. 2E).
The proinflammatory cytokine concentrations within dendritic cell tissues showed a decrease as a result of the application of MPF and DP-MPF. DSS-induced colitis is associated with increased production of proinflammatory cytokines and chemokines. The impact of MPF and DP-MPF treatments on proinflammatory cytokine production was evaluated by measuring cytokine concentrations in supernatants from dendritic cell tissue slice cultures. Increased proinflammatory cytokine concentrations were observed in the DSS-treated group. In contrast, MPF and DP-MPF treatment significantly suppressed proinflammatory cytokines and chemokines in dendritic cell-derived tissue slices.
The levels of TNF-α, IL-1α, IL-1β, IL-3, IL-6, IL-9, IL-10, IL-12 (P40), IL-12 (P70), IL-13, IL-17A, G-CSF (granulocyte-macrophage colony-stimulating factor), GM-CSF (granulocyte colony-stimulating factor), and IFN-γ (interferon gamma) were significantly decreased. Furthermore, MPF and DP-MPF significantly suppressed the production of chemokines such as MIP-1α (macrophage inflammatory protein 1 alpha), MIP-1β (macrophage inflammatory protein 1 beta), and eotaxin in dendritic cells.
The study showed that fucoidan extracts MPF and DP-MPF triggered and regulated cellular processes, significantly reducing oxidative stress and inflammation in a DSS-induced colitis model. In particular, the disease severity index, macroscopic and histological findings were strongly correlated with the reduction in inflammatory cytokines, reduced oxidative stress markers, and increased levels of SOD and CAT antioxidant enzymes. This study also demonstrates for the first time that Macrocystis pyrifera extracts MPF and DP-MPF possess potent anti-inflammatory and antioxidant effects in a DSS-induced colitis model. Additional preclinical research is necessary in animal models of DSS-induced colitis to thoroughly investigate and clarify the complex molecular mechanisms regulated by both MPF and DP-MPF.
Source: Pharmaceutics. 2022 Nov; 14(11): 2383. doi: 10.3390/pharmaceutics14112383
