Asthma, a chronic condition affecting the airways, is characterized by an increased responsiveness of the airways, inflammation within the airways, and changes in the structure of the airways themselves, all of which contribute to the overall disease process. The cycle of airway inflammation causes damage to the epithelium, changes in the smooth muscle (proliferation or atrophy), increased mucus production from secretory cells, ultimately leading to airway hyperresponsiveness, remodeling, impaired lung function, and breathlessness. The clinical treatment of asthma, while constantly undergoing revision and updates to improve efficacy, is unfortunately accompanied by various side effects that patients must consider.
In contrast to other findings, previous in vitro and ex vivo studies have shown that oligofucoidan possesses the ability to improve allergic immune responses and reduce the levels of inflammation in the airways.
In this blog, I would like to share highlights of the study, “Effects of oligo-fucoidan on the immune response, inflammatory status, and pulmonary function in patients with asthma: a randomized, double-blind, placebo-controlled trial” by Chia-wei Yeh et al. The goal of the study was to determine the impact of oligofucoidan on the immune status, inflammation, and pulmonary function of individuals with asthma.
First, twenty asthma patients were randomly divided into two groups: (1) the control group: receiving usual asthma treatment and placebo supplementation; (2) the fucoidan group: receiving usual asthma treatment and oligofucoidan supplementation. Pulmonary function tests, “Asthma Management Questionnaire” surveys, biochemical data, inflammatory factors, and immune cell subtypes were detected. During the treatment period, the levels of white blood cell count (p = 0.038) and creatinine (p = 0.012 and p = 0.008 at weeks 12 and 24, respectively) significantly decreased in the fucoidan group. Regarding lung function, the change in FEV1/FVC at week 4 in the group taking oligofucoidan was significantly greater than the change at week 4 in the control group. The study also showed that total IgE levels were reduced at weeks 12 and 24 in the oligofucoidan group, compared to the control group.
Surface antigen markers of immune cells (CD3CD4, CD3CD8, CD4CD25, IFN, CD4IFN, CD4IL-4, CD4IL-17, CD4FoxP3) were measured by flow cytometry at baseline, 4 weeks, 12 weeks, and 24 weeks of fucoidan supplementation, for the percentage of IFN+ cells in asthma patients after fucoidan supplementation. The fucoidan group showed significantly higher percentages of IFN+ and CD4+IFN+ cells after 24 weeks, while other immune cell subsets remained largely unchanged.
A significant decrease in the proportion of CD3+CD4+ cells was observed in the fucoidan group at week 12, when compared to the control group. In addition, the proportion of CD3+CD8+ cells was significantly decreased in the fucoidan group at week 4 compared to the control group. However, the proportion of IFN+ and CD4+IFN+ cells was more significantly increased at weeks 4, 12, and 24 in the fucoidan group compared to the control group.
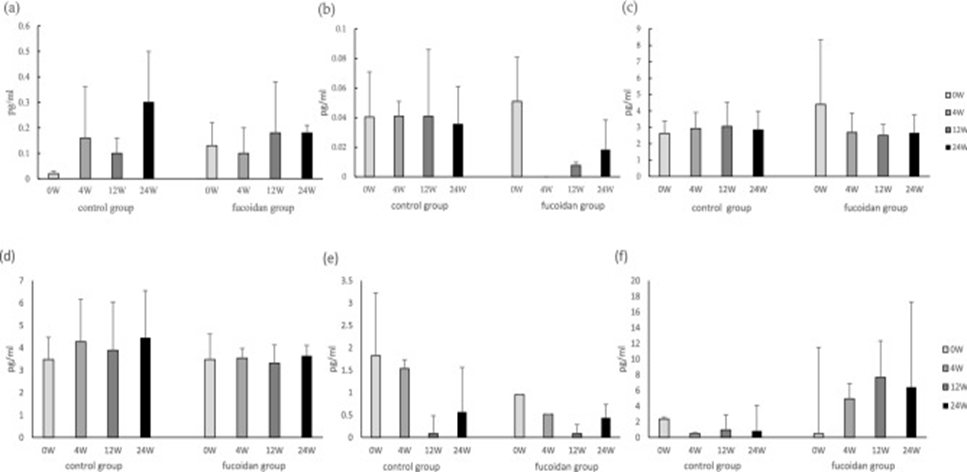
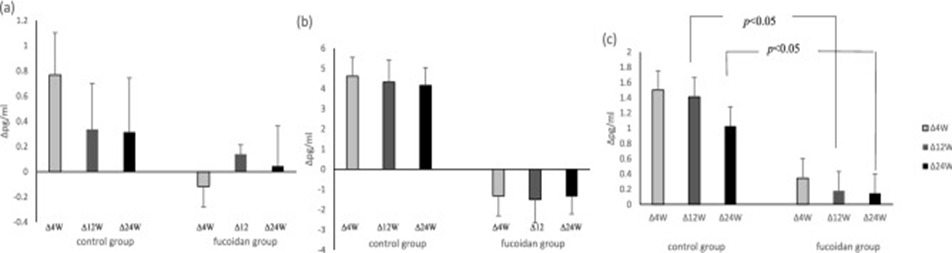
The levels of cytokines, including IL-1β, IL-4, IL-8, IL-6, IL-17, and IFN-γ, were analyzed using ELISA (Figure 1). There was no statistically significant difference in cytokine levels between the two groups during the treatment period. The alterations in cytokine levels observed in the two groups during treatment are presented in Figure 2. The results showed that the levels of IL-1β and IL-6 tended to decrease at 24 weeks in the fucoidan group compared to the control group, and in particular, the levels of IL-8 were significantly decreased at 12 and 24 weeks in the fucoidan group compared to the control group.
To conclude, the findings suggest that Oligofucoidan may have a beneficial effect on asthma by reducing the proportion of lymphocytes and the concentration of inflammatory factors, thereby suppressing respiratory inflammation and improving lung function in affected patients.
Source: Sci Rep. 2022 Oct 28;12:18150. doi: 10.1038/s41598-022-21527-3
