Diabetes poses a considerable and growing threat to global human health, as its incidence continues to rise internationally, demanding increased attention to prevention and treatment strategies. Although current medications reduce diabetes mortality and morbidity, their adverse health effects are becoming an urgent issue. In contrast, supplementing with polysaccharides provides an effective, side-effect-free approach to managing chronic diseases. The beneficial protective effects of Fucoidan from Laminaria japonica (LJF) on type 2 diabetes mellitus (T2DM) may be associated with the modulation of gut microbiota and metabolites, such as increasing Lactobacillus and Allobaculum. Therefore, in this blog, I would like to introduce the following study, “Fucoidan from Laminaria japonica Ameliorates Type 2 Diabetes Mellitus in Association with Modulation of Gut Microbiota and Metabolites in Streptozocin-Treated Mice” by Chenxi Zhang et al.
First, T2DM mice were divided into four groups: (i) model group (DM), orally administered normal water; (ii) metformin treatment group (ME), orally administered ME at 200 mg/kg body weight; (iii) LJF high-dose group (HF), orally administered LJF 500 mg/kg body weight; and (iv) LJF low-dose group (LF), orally administered LJF 150 mg/kg body weight. Weekly monitoring of body weight and FBG was conducted. Liver weight was determined, and this was used to calculate the liver weight to body weight ratio.
The diabetic group (DM) consumed more food and beverages post-streptozotocin (STZ) treatment but still lost weight. There was no difference in food intake between the LF/HF and DM groups, but food intake decreased in the ME group. The LF, HF, and ME groups weighed more than the DM group; however, there was no difference in weight between the LF, HF, and ME groups themselves. Oral glucose tolerance test (OGTT) results showed that blood glucose levels were higher in the DM group than in the NC group, reaching the maximum value at 15 min. Blood glucose levels in normal mice returned to baseline rapidly, while those in the DM group decreased gradually.
However, blood glucose reduction was more rapid in mice consuming LJF or ME; the impact of LJF was dose-dependent. The AUC level was higher in the DM group than in the NC group, and LJF reduced the AUC level in T2DM mice, which was higher than that in the ME group. The FBG level was higher in the DM group than in the NC group, and LJF dose-dependently reduced the FBG level in T2DM mice. These results indicate that LJF can be used as a prebiotic agent to alleviate the typical symptoms of T2DM.
The T2DM mice receiving LJF exhibited dyslipidemia, with elevated serum TG, LDL-C, TC, ALT, AST, and FFA, and decreased GLP-1 and HDL-C, when compared to the non-diabetic control group. In contrast, low- and high-dose LJF decreased the serum LDL-C, TC, AST, TG, ALT, and FFA contents, and increased the HDL-C and GLP-1 levels in T2DM mice. These findings indicate a significant improvement in lipid metabolism abnormalities in mice with type 2 diabetes mellitus (T2DM) following LJF treatment.
Liver weight and liver indexes for liver glycogen content and oxidative stress were increased, and liver glycogen was decreased in the DM group compared with the NC group. LJF dose-dependently decreased liver weight and liver indexes in T2DM mice. SOD, CAT, and T-AOC contents were decreased, and MDA levels were increased in the DM group compared with the NC group. The administration of high doses of LJF to T2DM mice produced a decrease in MDA levels and a simultaneous increase in T-AOC and SOD levels, whereas low doses of LJF resulted only in a reduction of MDA levels. Histological analysis showed that high doses of LJF reduced fat accumulation in T2DM mice.
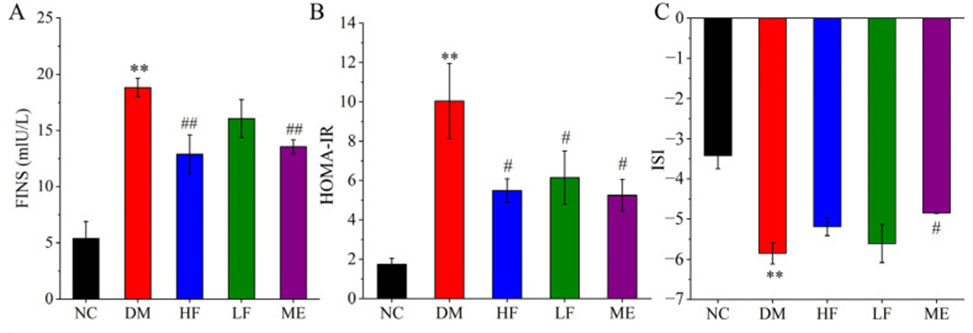
As shown in Figure 1A, LJF modulated insulin resistance and sensitivity. The DM group exhibited elevated FINS levels compared to the NC group, while LJF treatment dose-dependently lowered FINS in T2DM mice. The DM group showed elevated HOMA-IR and decreased ISI, revealing the imbalance between insulin resistance and insulin sensitivity (Figure 1B, C). High doses of LJF reduced HOMA-IR levels and increased ISI levels in T2DM mice, whereas low doses of LJF did not affect ISI levels. This suggests that the effect of LJF on insulin resistance and insulin sensitivity imbalance may be in a dose-dependent manner. Low and high doses of LJF attenuated islet necrosis and β-cell damage, and the latter appeared to have a better protective effect on islets. These findings indicate that LJF may safeguard islets and correct the imbalance of insulin resistance and sensitivity, thereby improving the dysregulation of insulin-glucose metabolism in diabetic mice.
The DM group showed lower concentrations of SCFAs—acetate, butyrate, propionate, isobutyrate, isovalerate, and valerate—than the NC group. In contrast, high-dose LJF increased the production of acetate, propionate, i-butyrate, i-valerate, and valerate in T2DM mice, and low-dose LJF increased the contents of acetate, valerate, and i-valerate. The administration of ME to T2DM mice resulted in elevated levels of several SCFAs (acetate, butyrate, propionate, isobutyrate, isovalerate, and valerate). High-dose LJF had a comparable impact, with the exception of butyrate, potentially due to overlapping mechanisms of gut microbiota modulation.
The effects of LJF and ME on gut microbiota in T2DM mice differed: LJF specifically reduced Proteobacteria, while ME altered the levels of Proteobacteria, Firmicutes, and Bacteroidetes, decreasing the Firmicutes-to-Bacteroidetes ratio, highlighting their specific modulatory effects.
This study’s findings indicate that LJF, a microbial metabolite, plays a crucial role in type 2 diabetes remission by significantly impacting amino acid, glutathione, glyoxylate, and dicarboxylate metabolic pathways. The findings of the study suggested the potential of LJF to serve as a prebiotic agent, thereby offering a preventative and therapeutic approach to type 2 diabetes. However, further research is needed into key gut bacteria and their regulatory mechanisms before the LJF approach can be applied.
Source: Foods. 2023 Jan; 12(1): 33. doi: 10.3390/foods12010033
