The combination of complementary and alternative medicines (CAM) with conventional cancer therapies has become a popular approach. However, there is a lack of clinical evidence supporting their safety when used alongside conventional treatments. Investigating the effects of CAM on conventional drugs is necessary to generate evidence-based information regarding the safe combination of many of these drugs, including anticancer drugs.
In this blog, I would like to share the following study with you: “The Effect of Undaria pinnatifida Fucoidan on the Pharmacokinetics of Letrozole and Tamoxifen in Patients with Breast Cancer” by Shreya Tocaciu et al.
The study consisted of 20 patients, with an equal distribution of 10 females taking letrozole and 10 females taking tamoxifen. The median age of participants was 59 years, with a range of 43 to 76 years. A variety of subjective adverse events were self-reported, including nausea, diarrhea, constipation, and headache. All were mild and transient. In contrast, four patients who were part of the study reported a decrease in bone and muscle pain while undergoing the three-week fucoidan treatment. Among these patients, two were on letrozole and the other two were on tamoxifen. During the study period, blood parameters did not change significantly in all patients, except for one. Before fucoidan treatment, this patient’s liver function test (LFTs) showed mild abnormalities (gamma-glutamyltransferase 140 units). After three weeks of taking Undaria pinnatifida fucoidan, Gamma-glutamyl transferase (GGT) levels remained elevated (174 units). The cause of the elevated GGT levels was unknown, and specifically, there was no evidence of liver metastases.
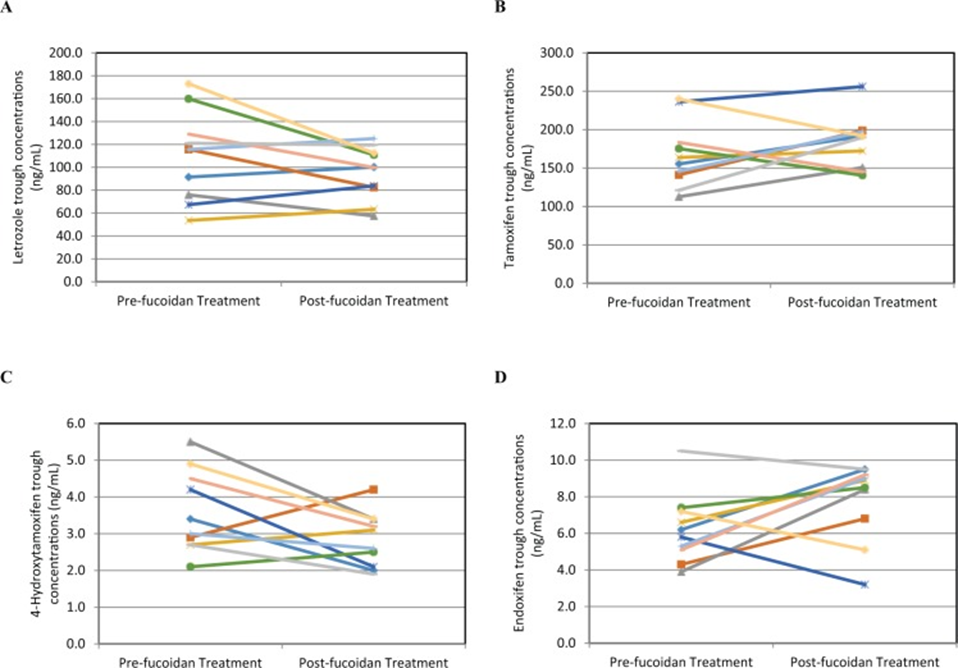
The study found that the combination of wakame fucoidan did not have a substantial impact on the steady-state trough plasma concentrations of letrozole and tamoxifen hormone therapies in breast cancer patients. In addition, no significant differences were observed in the plasma concentrations of tamoxifen’s active metabolites, 4-hydroxytamoxifen, and endoxifen, before and after fucoidan administration. However, 4-hydroxytamoxifen concentrations decreased by an average of 21% and endoxifen concentrations increased by an average of 25% after fucoidan administration, as shown in Figure 1. 4-hydroxytamoxifen and endoxifen are significantly more potent than tamoxifen. The long-term advantages of tamoxifen therapy in breast cancer are thought to be directly linked to the maintenance of endoxifen plasma concentrations above a specific threshold. Although the changes in endoxifen concentrations after fucoidan intake were not statistically significant, further investigations are needed to confirm whether the observed increase in plasma concentrations has clinical implications.
There is no proof indicating that fucoidan has any impact on the drug-metabolizing enzymes that metabolize letrozole or tamoxifen. However, it is worth noting that letrozole is metabolized by Cytochrome P450 2A6 (CYP2A6) and tamoxifen is metabolized by Cytochrome P450 2D6 (CYP2D6). Genetic variations in these genes can lead to variations in how these compounds are metabolized. Large interpatient variability in drug and metabolite concentrations was observed, which is consistent with other pharmacokinetic studies of letrozole and tamoxifen. Fucoidan was not systematically tested against Cytochrome P450 (CYP) enzymes, and the limited evidence from the small sample size of this study did not demonstrate an effect on CYP enzymes.
In conclusion, the administration of Undaria pinnatifida fucoidan did not significantly affect steady-state trough concentrations of letrozole or tamoxifen and was well tolerated. Additionally, there were no reported adverse effects of fucoidan, and the monitoring of toxicity did not reveal any significant differences in the measured parameters throughout the study duration. These results suggest that fucoidan in the form and dose studied can be administered concomitantly with letrozole and tamoxifen without the risk of clinically significant interactions.
Source: Integr Cancer Ther. 2018 Mar; 17(1): 99–105. doi: 10.1177/1534735416684014
