Neutrophils play a crucial role in every stage of both human and experimental abdominal aortic aneurysm (AAA) development. The initial step in this process involves the rolling and entrapment of neutrophils within the intraluminal thrombus (ILT), which is considered to be the primary process mediated by P-selectin, expressed by activated platelets. In this blog, I would like to introduce you to the study, “Fucoidan interferes with Porphyromonas gingivalis-induced aneurysm enlargement by decreasing neutrophil activation” by Jean-Marc Alsac MD et al,. In the study, the researchers evaluated the beneficial effects of fucoidan, which is a competitive binder of P-selectin, on the growth of aneurysms in a rat model of the aortic aneurysm. This model involved the induction of neutrophil enrichment in ILT (intra-luminal thrombus) through repeated weak bacteremia.
In the first step, a group of sixty Lewis rats with experimental AAA was created using decellularized aortic xenografts. Subsequently, these rats were divided into four groups, with two groups serving as controls. In the fucoidan control (FC) group, a 200 mg dose of fucoidan (F) was administered, while group C was given saline instead of fucoidan. He also gave two groups weekly injections of Porphyromonas gingivalis (Pg). Group F+Pg received 200 mg of intraperitoneal fucoidan, and group Pg received saline. AAAs were harvested 4 weeks later, and peripheral blood was sampled. Concentrations of cell-free DNA (cf-DNA) and myeloperoxidase (MPO) antigen were assessed in plasma and media conditioned by AAA. Histological analysis and P-selectin immunostaining were carried out on the AAA tissue samples.
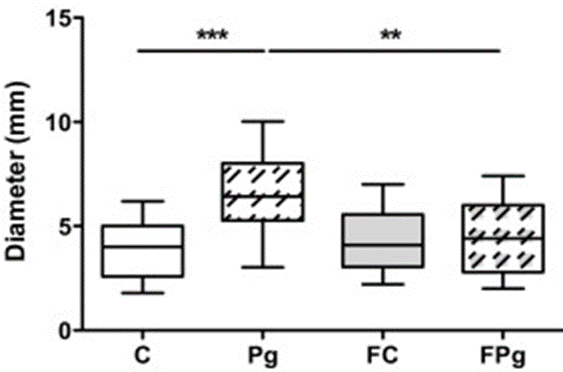
Figure 1 demonstrates that the injection of P. gingivalis led to a substantial increase in the maximum diameter of the aneurysms, when compared to the control group of rats that received saline injections.
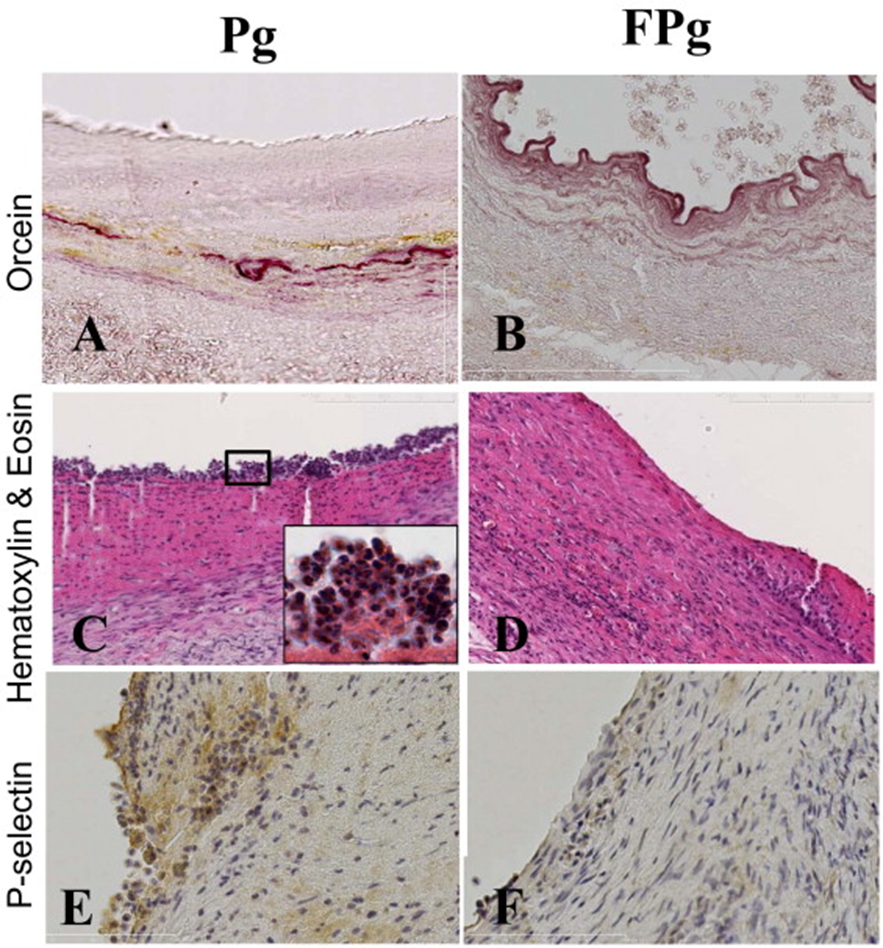
The administration of fucoidan to rats resulted in a decrease in aneurysm diameter, whereas rats injected with Pg did not show this reduction. In the histological analysis of AAA, it was observed that fucoidan led to a decrease in the thickness of ILT in rats injected with Pg. Furthermore, there were fewer trapped neutrophils and signs of a healing process, similar to what was seen in the control group C. The luminal surface of aneurysms in fucoidan-treated rats compared with other groups suggests an interaction between fucoidan and P-selectin. Fucoidan treatment effectively decreased MPO concentrations in both plasma and conditioned media of Pg-injected rats, demonstrating the inhibition of ILT’s biological activity. Fucoidan treatment led to a decrease in neutrophil activation and cell death, resulting in a significant reduction in the concentration of cf-DNA in both the plasma and conditioned media of the rats.
The use of an intraperitoneal osmotic pump is necessary to prove that fucoidan can effectively hinder interactions between thrombus, neutrophils, and bacteria. This pump will ensure a continuous release of 200 mg of fucoidan over the course of the 4-week experiment. The rats injected with P. gingivalis were divided into two groups, and the rats that received 200 mg of fucoidan during the 4-week experiment exhibited reduced aneurysm diameters, indicating the inhibition of aneurysm growth. The immunostaining results from Figure 2 indicate that fucoidan treatment leads to a reduction in P-selectin on the luminal surface of the aneurysmal aortic wall, suggesting an interaction between fucoidan and P-selectin.
Additionally, fucoidan seems to have localized effects on the activation of neutrophils in ILT at the AAA level. The research demonstrated a clear link between the interaction of fucoidan treatment and P. gingivalis-induced neutrophil activation, leading to changes in AAA diameter and MPO concentration in both the conditioned medium and conditioned medium. Plasma, like cf-DNA found in conditioned media, does not correlate with circulating neutrophil counts or plasma cf-DNA levels. This suggests that fucoidan primarily affects ILT levels instead of exerting systemic effects on neutrophils. This indicates a more distinct outcome.
Chronic bacteremia can lead to subclinical infections of various cardiovascular tissues, including thrombus in AAA. P. gingivalis is a completely anaerobic bacterium and cannot grow within wall thrombi. Hence, while it may not be a potent pathogen in isolation, it does lead to the activation of neutrophils, which hampers the healing of an aneurysm.
The healing process, which involves the colonization of mesenchymal cells in the aneurysm wall, typically takes place without any additional damage. However, this restorative process is not observed in human evolutionary AAAs, which is why it is commonly studied in experimental AAAs in small animals. It has been thought that this is a limitation. The weak pathogens, particularly P. gingivalis, may contribute to the limitation in treating human AAA, as evidenced by the fibrous scarring of the aneurysm wall and the recurrent increase in neutrophils in the ILT. You can think of it as a goal for the wall to achieve. These findings indicate that fucoidan can cause a reversal effect on the degeneration of experimental aneurysms by decreasing neutrophil activity in ILT that is dependent on Pg.
Therefore, fucoidan could be considered as a potential treatment for AAA since it can decrease the activation of neutrophils, which are involved in the degenerative process of aneurysm expansion and rupture.
Source: PMID: 23141684 DOI: 10.1016/j.jvs.2012.07.039
