Radiation therapy (RT) is widely recognized as a significant treatment option for numerous cancer types. However, it is important to acknowledge that it can result in the development of radiation pneumonitis (RP). Radiation pneumonitis is a type of pneumonia caused by damage to the lungs caused by radiation therapy for cancer in the chest (lung cancer, esophageal cancer, breast cancer, malignant lymphoma, etc.). It especially causes damage to cells in the alveoli and lung blood vessels. According to reports, when DNA in injured cells undergoes damage, it is said to contribute to the development of this condition, causing these cells to release substances like cytokines that induce inflammation. As a result of inflammation primarily affecting the pulmonary interstitium, the body initiates the process of pulmonary fibrosis as a means of repair.
Fucoidan, a type of sulfated polysaccharide, is primarily derived from different varieties of seaweed. Recent studies have proven the anti-inflammatory effects of fucoidan. However, no studies have reported well-established prophylactic agents for RP. Therefore, in this blog, I would like to introduce the contents from the research, “Fucoidan Inhibits Radiation-Induced Pneumonitis and Lung Fibrosis by Reducing Inflammatory Cytokine Expression in Lung Tissues” by Hsin-Hsien Yu et al., on the effects of fucoidan on RP and radiotherapy (RT)-induced pulmonary fibrosis.
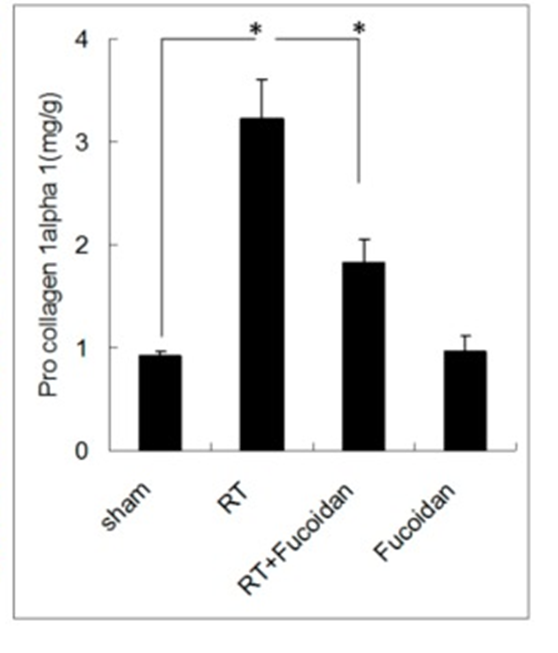
The objective of the study was to investigate the effects of fucoidan on RP-induced and radiotherapy (RT)-induced pulmonary fibrosis. The effects of fucoidan administration (200 mg/kg/day, gavage for 14 days) on RP-induced fibrosis and radiotherapy were examined in lung tissue specimens from irradiated (10 Gy/shot) C57BL/6 mice. First, the COL1A1 gene produces a component of type I collagen called procollagen 1 alpha. Therefore, the entire left lobe of the lung was homogenized to measure procollagen 1α levels by ELISA. (See Figure 1, right panel)
Analysis of the ELISA results indicated that the RT group displayed higher levels of collagen deposition, while the RT + fucoidan group exhibited lower levels of collagen deposition. Quantitative results of procollagen 1 alpha showed that RT significantly enhanced collagen formation in lung tissue. Also, the collagen levels in the RT + fucoidan group (1.83 ± 0.23 mg/g) fucoidan administration significantly decreased collagen formation in lung tissue. These results indicated that fucoidan attenuated RT-induced pulmonary fibrosis in irradiated mouse lung tissue.
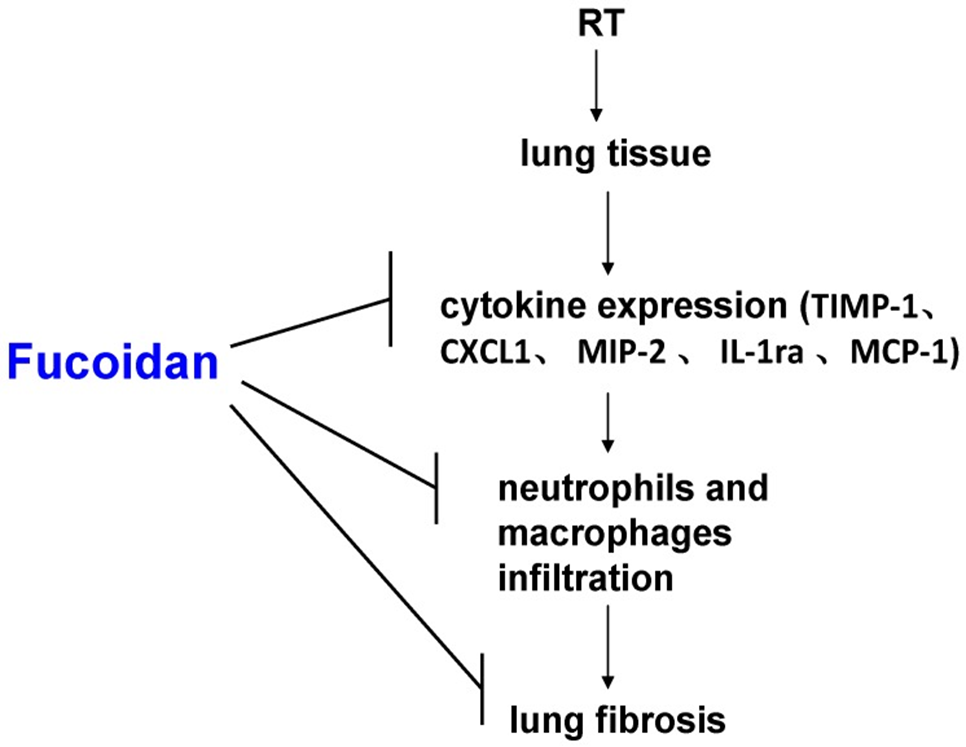
Cytokine expression patterns in pleural effusions were determined using cytokine arrays and confirmed by enzyme immunoassay. As a result, fucoidan administration attenuated RP- and RT-induced fibrosis in lung tissue. The researchers observed a decrease in the accumulation of neutrophils and macrophages in the irradiated lung tissue. This decrease helped to reduce the severity of radiation-induced pulmonary fibrosis, as evidenced by the results from Masson’s trichrome staining. They analyzed the expression pattern of inflammatory cytokines in irradiated pulmonary pleural effusions by means of protein arrays. Thus, it was revealed that the administration of fucoidan induced a shift in the expression pattern of inflammatory cytokines in irradiated lung tissue. The expression levels of TIMP-1, CXCL1, MCP-1, MIP-2, and interleukin-1Ra were significantly elevated in the pleural effusion. Notably, fucoidan administration contributed to a significant decrease in their expression. Fucoidan has the ability to modify the expression pattern of pro-inflammatory cytokines, resulting in a reduction of RP- and RT-induced pulmonary fibrosis.
In the present study, the administration of fucoidan to irradiated mice resulted in the reduction of cytokine expression (TIMP-1, CXCL1, MCP-1, MIP-2, and IL-1Ra) in the pleural effusion collected, as well as the fibrosis. It was demonstrated that pleural effusion-induced collagen expression in blasts was reduced. It correlated with decreased neutrophil and macrophage infiltration in lung tissue. Infiltration of macrophages and neutrophils can lead to RP- and RT-induced pulmonary fibrosis. (See Figure 2) This finding may contribute to the facilitation of fucoidan-based therapeutic strategies in the prevention of RP in clinical settings.
In conclusion, fucoidan has the potential to modify the expression pattern of pro-inflammatory cytokines, leading to a reduction in RP- and RT-induced pulmonary fibrosis. Hence, Fucoidan could be a potential therapeutic agent for the reduction or prevention of RP.
Source: Mar Drugs. 2018 Oct; 16(10): 392. doi: 10.3390/md16100392
