In this blog, I would like to share the study “Fucoidan inhibition of lung cancer in vivo and in vitro: role of the Smurf2-dependent ubiquitin-proteasome pathway in TGFβ receptor degradation” by Hsien-Yeh Hsu et al. There are many significant types of research on fucoidan and cancer. However, this study is conducted for the first time with a new mechanism of fucoidan’s anti-tumor activity, namely by modulating the TGFR/Smad7/Smurf2-dependent axis. Furthermore, the study observes that fucoidan reduces tumor growth, resulting in TGFR protein degradation and inhibition of lung cancer cell progression in vitro and in vivo.
Transforming growth factor-β (TGFβ) receptor (TGFR) plays a crucial role in regulating growth and progression, and high expression of TGFRI in lung cancer specimens is associated with poor prognosis.
The study showed that a novel mechanism of fucoidan’s anti-tumor activity by modulating the TGFR/Smad7/Smurf2-dependent axis reduced tumor growth and decreased TGFR protein degradation and progression of lung cancer cells in vitro and in vivo. It was the first to identify it as a hindrance. Their current findings hold promise for fucoidan as a potential lung cancer therapeutic or dietary supplement, acting via Smurf2-dependent ubiquitinolysis of TGFβ receptors.
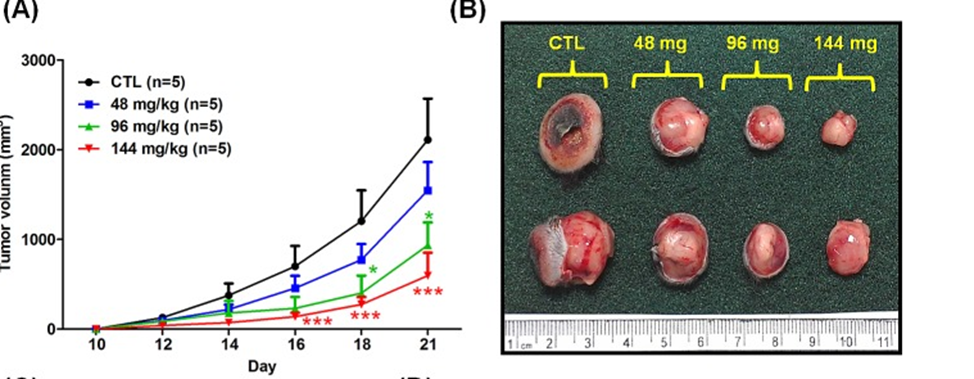
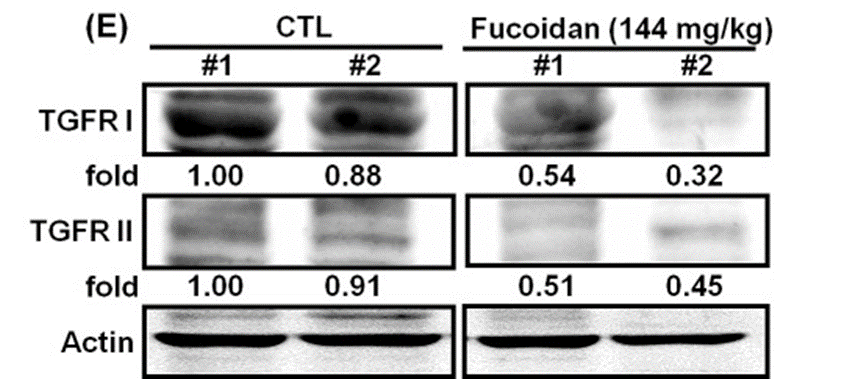
First, LLC1 cells were inoculated subcutaneously in the back of male C57BL6 mice, and tumor growth rates were assessed over 21 days. Fucoidan-fed mice showed a marked dose-dependent reduction in tumor volume and tumor weight. (See Figures 1A and 1B) In contrast, little weight difference in the mouse was observed between the fucoidan-fed mice and the ddH2O control group. Western blot analysis was used to validate TGFR expression in tumor lesions. The study found that LLC1-fed mice with fucoidan expressed fewer TGFRs (TGFRI and II) than the control group. (See Fig. 1E) Thus, showing that fucoidan downregulates the TGFRI and TGFRII protein expression in tumor lesions in vivo. These results indicate that fucoidan suppresses tumorigenesis and reduces TGFR protein expression in an LLC1-bearing mouse model in vivo.
Later, in TGFR function related to tumorigenesis, fucoidan promotes Smurf2 and Smad7 binding to TGFR and degradation of TGFR via the Smurf2-dependent ubiquitin-proteasome pathway (UPP). Therefore, the current findings suggest that fucoidan has excellent potential as a therapeutic intervention in the control of lung cancer and that manipulating Smurf2-dependent UPP-mediated degradation of TGFR proteins may be effective for cancer patients. It shows that it may be an excellent approach.
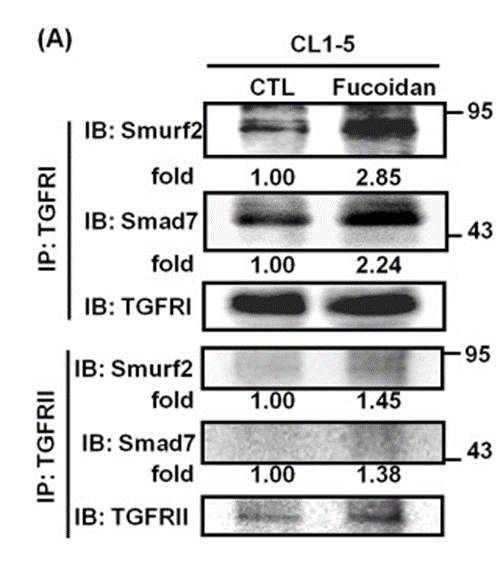
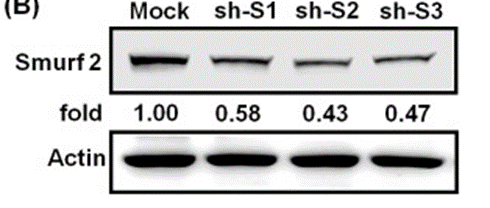
Smurf2 is one of the essential E3 ligases in regulating TGFR expression. On the other hand, the adapter protein Smad7 has a crucial function in facilitating her Smurf2 binding on TGFRI and contributes to TGFR heterocomplex disassembly. Hence, this study mainly investigated whether Smurf2 and Smad7 are involved in the processing steps of fucoidan-mediated UPP degradation of TGFR in lung cancer cells. Figures 2A and 2B show that during fucoidan treatment of CL1-5 cells, the amounts of Smurf2 and Smad7 proteins bound to TGFRI and TGFRII in fucoidan-treated patients cells were doubled and 1-fold, respectively, compared to control cells and significantly increased. These results suggest that Smurf2 and Smad7 may be involved in fucoidan-enhanced ubiquitin-dependent TGFR degradation.
In conclusion, one of the mechanisms by which fucoidan suppresses lung cancer in vivo and in vitro may depend on Smurf2/Smad7-mediated promotion of TGFR ubiquitination and degradation. In TGFR function related to tumorigenesis, fucoidan promotes Smurf2 and Smad7 binding to TGFR and degradation of TGFR via the Smurf2-dependent ubiquitin-proteasome pathway (UPP). Hence, the current findings suggest that fucoidan has excellent potential as a therapeutic intervention in the control of lung cancer and that manipulating Smurf2-dependent UPP-mediated degradation of TGFR proteins may be effective for cancer patients. It shows that it may be a beneficial strategy.
Source: Oncotarget. 2014 Sep; 5(17): 7870–7885. doi: 10.18632/oncotarget.2317
