Obesity, including excessive body fat accumulation, is closely associated with the development of cardiovascular disease, insulin resistance (IR), Type 2 diabetes, and non-alcoholic fatty liver disease (NAFLD). Hypertrophic adipocytes also secrete adipokines such as adiponectin, leptin, tumor necrosis factor-α (TNF-α), and interleukin-6 (IL-6), which are known to alter insulin activity in adipose tissue, liver, and muscle. Additionally, obesity induces chronic inflammation, leading to elevated metabolic dysfunction such as IR, NAFLD, and cardiovascular disease. It indicates that inflammation is a significant contributor to the pathogenesis of obesity and its associated metabolic dysfunctions.
On the other hand, in previous studies, fucoidan was investigated for its anti-oxidative, antitumor, and anti-inflammatory effects, including the prevention of hypertension associated with obesity. However, it is still unclear whether fucoidan affects adipose tissue distribution (visceral and subcutaneous fat) and inflammation.
Thus in this blog, I would like to share the study, “Fucoidan antagonizes diet-induced obesity and inflammation in mice” by Lei Wang et al. The study used fucoidan in HFD (a high-fat diet) fed mice to investigate its anti-obesity potential.
First, eight-week-old male mice were fed HFD or chow (CD) for 24 weeks. Then, Fucoidan administration to male mice was initiated after eight weeks of feeding (CD or HFD). Mice were given fucoidan (Fucus vesiculosus) intraperitoneally at 10 mg/(kg·day) daily for 16 weeks.
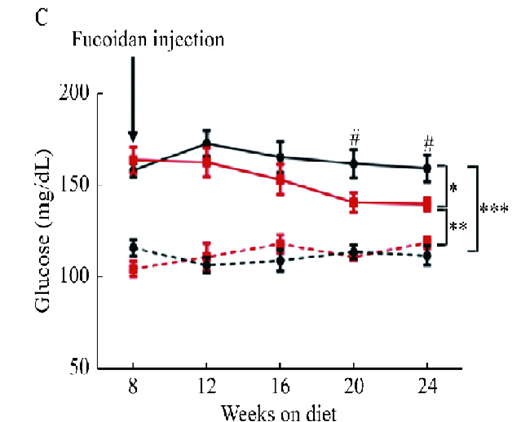
Fucoidan was continuously administered to mice of HFD feeding, and changes in body weight and blood glucose level were examined. After eight weeks of fucoidan administration (from the 16th week of HFD feeding), the body weight of the mice decreased but not in CD-fed mice. After receiving fucoidan treatment, hypoglycemic effects were shown in HFD mice. (See Figure 1C) Fucoidan administration also significantly improved insulin sensitivity in HFD mice after fucoidan treatment. Moreover, fucoidan-treated mice showed reduced plasma FFAs, triglycerides, and cholesterol compared to HFD-fed control mice.
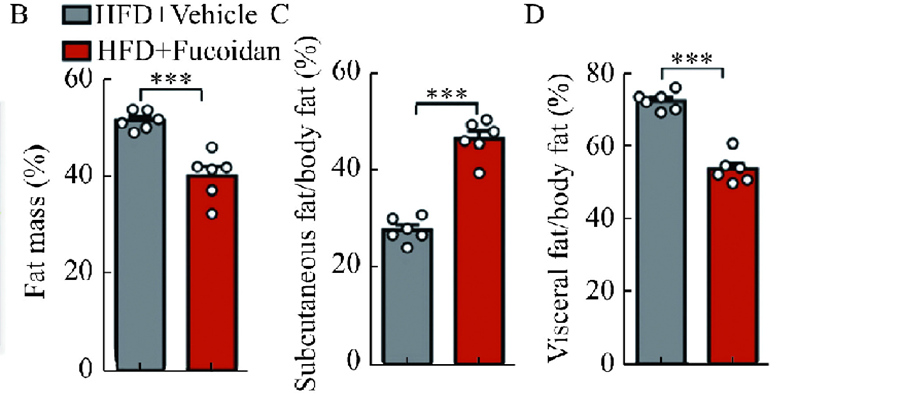
Next, they used a micro-CT system to examine mice’s visceral and subcutaneous fat mass. Administration of fucoidan significantly decreased the percentage of body fat and visceral fat. It increased the rate of subcutaneous fat, which some subcutaneous fat is good for your body and helps protect your skin. (See Figure. 2B) Epididymal fat, a type of visceral fat, was also reduced by fucoidan treatment. (See Figure. 2D)
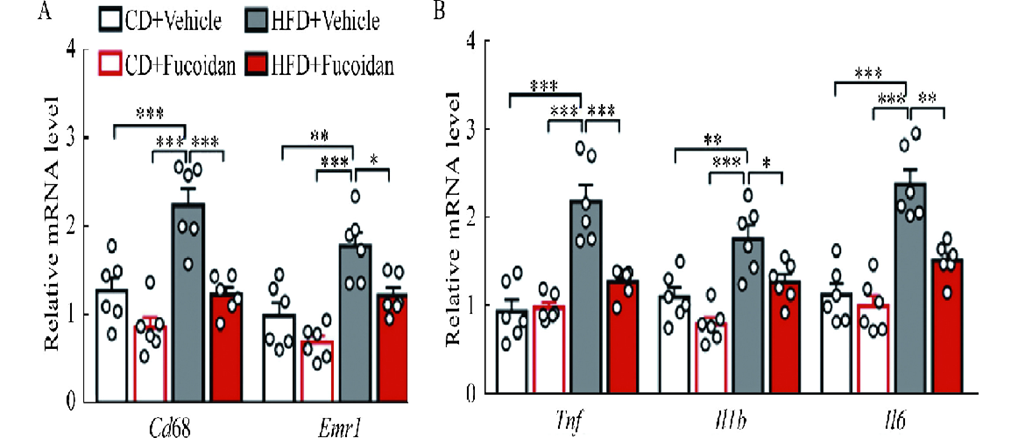
Chronic inflammation of fat plays an essential role in developing obesity and obesity-induced diseases. It was observed that the expression levels of Cd68 and Emr1, significant markers of inflammatory cells in epididymal adipose tissue, were reduced in fucoidan-treated HFD mice. (See Figure. 3A) Additionally, the expression of proinflammatory cytokines (Tnf, Il1b, and Il6) was decreased in fucoidan-treated mice. (See Figure. 3B)
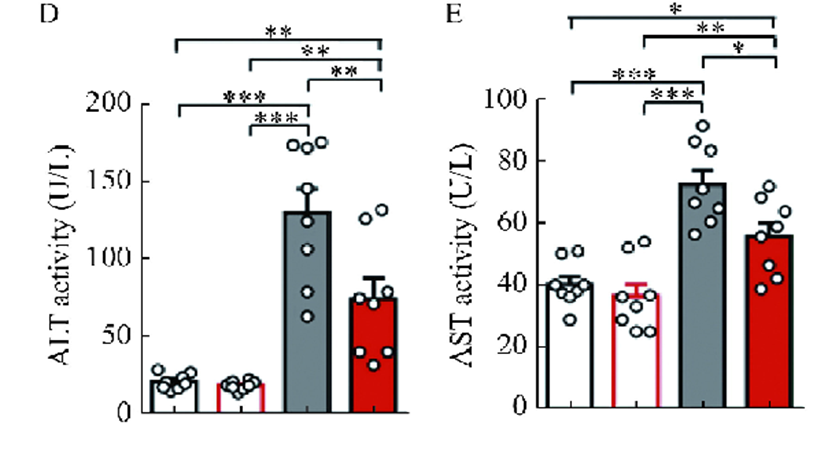
Excessive energy intake can lead to lipid deposition in adipose tissue and the liver, accelerating the progression to steatohepatitis, a severe complication of obesity. It was found that the liver weight decreased with decreasing levels accompanied by reduced levels of hepatic triglycerides and cholesterol. Fucoidan treatment also reduced liver injury in HFD-fed mice. (See Figure. 3D E) Histological examination of the liver confirmed that the hepatic lipid droplets induced by HFD feeding were dramatically reduced by fucoidan treatment.
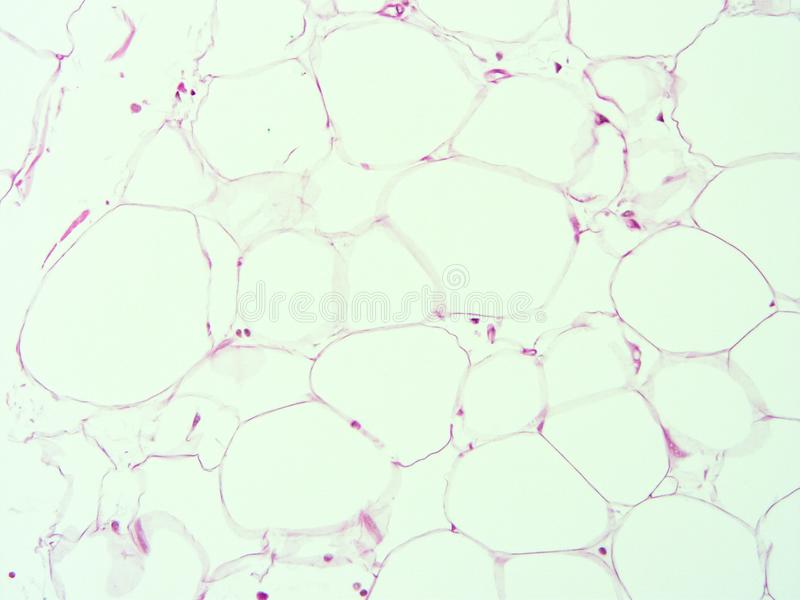
In the mentioned study, the reduction in fat mass was accompanied by a decrease in adipocyte diameter and inhibition of anti-adipogenic effects in fucoidan-treated HFD mice. In conclusion, promoting adipogenesis may be the process by which fucoidan prevents obesity and metabolic dysfunction.
They also show that fucoidan suppresses body fat accumulation and HFD-induced fat inflammation in mice. Hence, with previous combined studies proving that fucoidan suppresses obesity-related hypertension, fucoidan may be used as a new anti-obesity agent. However, further research on efficacy in humans is needed in the future.
Source: J Biomed Res 2021 May; 35(3): 197–205. doi: 10.7555/JBR.34.20200153