Helicobacter pylori is a bacterium discovered in the 1980s that commonly inhabits the stomach and causes damage to the mucous membranes. Helicobacter pylori are closely related to the development of gastric ulcers (gastric ulcers and duodenal ulcers). It is believed that infection with Helicobacter pylori causes atrophic gastritis, which leads to gastric cancer. This condition is usually treated with antibiotics used to inhibit or kill pylori effectively. It significantly reduces the incidence of gastric adenomas and cancer. Unfortunately, H. pylori have developed drug resistance to many clinically used antibiotics over the years. It also highlights the danger of antibiotic failure during pylori treatment.

On the other hand, there have been significant studies on fucoidan, a sulfated polysaccharide extracted from the Sargassum hemiphyllum that can significantly reduce the infection of H. pylori without developing drug resistance. So in this blog, I would like to share how fucoidan works on H. pylori through the study “Fucoidan from Sargassum hemiphyllum inhibits infection and inflammation of Helicobacter pylori” by Bo‑Rui Chen1 et al.
First, fucoidan toxicity was evaluated using RAW264.7 cells (monocyte/macrophage-like cells), including cytotoxicity to RAW264.7 but was not cytotoxic.
Further, to investigate fucoidan for NO (nitric oxide) inhibition, LPS was added to RAW264.7 cells to induce NO, and the NO production of the LPS-supplemented group was set to 100%. In contrast, LPS-induced NO production was measured in samples of RAW264.7 cells supplemented with various concentrations of fucoidan. The results showed that NO concentration was dose-dependently inversely proportional to the amount of fucoidan added to the cells. NO production reached a significant difference in cells at 250 μg / mL fucoidan compared to the LPS group. (See Fig. 1).
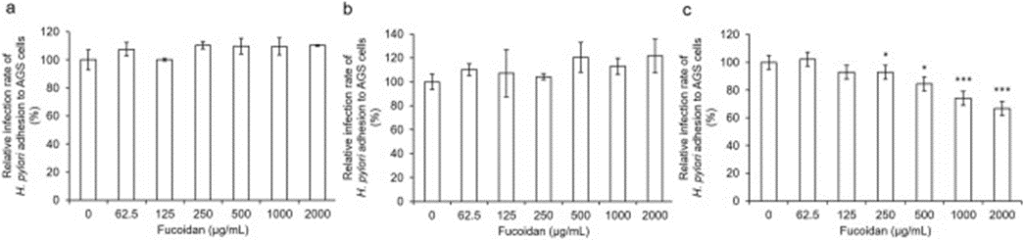
Next, the inhibitory activity of fucoidan during pylori infection was investigated. The infection rate of Helicobacter pylori to cells was set to 100: 1 (multiplicity of infection, MOI = 100). Our inspection consists of three test groups: post-treatment, pre-treatment, and collaborative treatment. Bacterial challenge experiments have shown that fucoidan is dose-dependently effective against Helicobacter pylori infection in the post-treatment group. The infection rate was significantly reduced at a 250 μg / mL fucoidan concentration compared to the untreated group. At a fucoidan concentration of 2000 μg / mL, the infection rate was further reduced to 40%.
There was no inhibitory activity in the other two groups (See Fig. 2), suggesting that fucoidan interacts directly with H. pylori.
Thus, to understand whether fucoidan regulates the immune response of H. pylori-infected mice, IL-4 and IL-5 expression levels were measured to see if they followed the Th2 pathway. It was found that the expression level of IL-4 was not significantly different between the test groups. However, IL-5 expression levels were positively correlated with the severity of eosinophil infiltration and were significantly reduced in the test group. When the expression levels of IL-6, IL-1β, and TNF-α were subjected to cytokine analysis, H. There was a dramatic increase in BALB / c mice infected with pylori for two weeks. On the contrary, IL-6 and TNF-α expression levels were significantly reduced in infected mice treated with fucoidan. Interestingly, only IL-1β was reduced considerably in the Post-Fu group.
The result shows fucoidan has an excellent protective effect against pylori infection overall. Fucoidan is effective in a position to protect the stomach from H. pylori infection by reducing both the total count of H. pylori and induced inflammation.