Proliferative vitreous retinopathy (PVR) is a condition that is worsened, by retinal detachment. In this condition, the neural retina is detached from the retinal pigment epithelial cells, and diabetic retinopathy leads to abnormalities in the retina’s blood vessels due to hyperglycemia.
If retinal detachment or diabetic retinopathy persists for a long time, or if the retinal detachment surgery does not entirely close the gap, fibrous cells increase on the retina’s surface and vitreous to heal the wound. The increased fibrous cells form a proliferative membrane between the vitreous and the retina. The proliferative membrane and vitreous shrink and pull the retina forward, causing the retina to detach and a particular type of retinal detachment.

It is stated that the success rate of surgery is lower than that of typical retinal detachment. Epithelial-Mesenchymal Transition (EMT) in retinal pigment epithelial (RPE) cells is known as one of the pathogenic mechanisms of RPV. EMT is a biological mechanism necessary for healing, such as retinal detachment and surgical laceration. It temporarily loses the characteristics of the mature epithelial system and induces conversion to mesenchymal cells with high proliferative and regenerative ability. However, Chronic inflammation repetition of the proliferative response in a persistent state causes abnormalities and causes fibrosis in the eye. Therefore, suppressing EMT in RPE cells is an effective way to prevent PVR.
So, in this blog, I would like to inform you if fucoidan, a sulfated polysaccharide, has an effect on RPV through the study “Protective effect of fucoidan on the epithelial-mesenchymal transition of retinal pigment epithelial cells and progression of proliferative vitreoretinopathy” by Yao Zhang et al. In some studies, fucoidan is reported to have preventive and ameliorating effects by suppressing EMT in renal interstitial fibrosis and diabetic nephropathy. Thus, they investigated the effects of fucoidan on EMT and the progression of PVR in RPE cells.
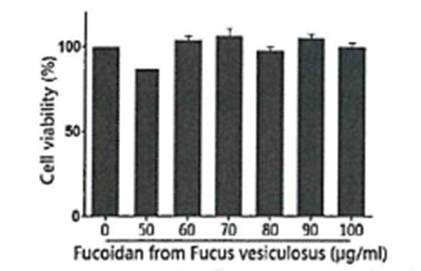
First, fucoidan derived from Fucus vesiculosus was added to RPE cells, and the state of the cells after 48 hours was observed. As a result, it was observed that there was no effect on cell viability and the toxicity of RPE cells was extremely low (Fig. 1). Next, RPE cells were cultured in the presence of TGF-β1, an EMT-inducing factor. The expression status of the epithelial marker E-cadherin, the mesenchymal marker smooth muscle α-actin (α-SMA), and fibroin was used as an index. And the effect of fucoidan on EMT was investigated. As a result, in the non-addition group, a decrease in E-cadherin and increased mesenchymal stem markers were observed in the presence of TGF-β1, and EMT was induced.
On the other hand, it was found that in the fucoidan-added group, the increase/decrease of each marker associated with TGF-β1 treatment was alleviated, and the appearance of EMT was not indicated. (Fig. 2). This result suggests that fucoidan acted to suppress EMT in RPE cells.
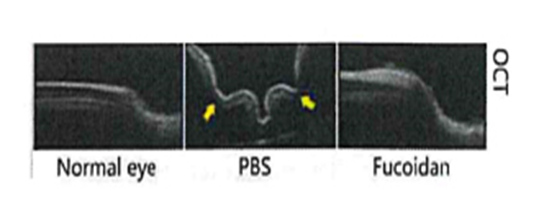
Finally, an animal model study inducing PVR in the rabbit’s right eye examined whether fucoidan effectively suppressed PVR progression. Prepare a group infused with fucoidan into the vitreous body and a control group infused with Phosphate-Buffered Saline (PBS). And they checked the progress of PVR in photographing the condition of the retina by a non-invasive imaging method called Optical Interference Tomography (OCP).
As the result of examining the progress of PVR, the control group treated with PBS developed extensive retinal detachment and retinal foramen, as seen in the arrow in the figure. In contrast, the group treated with fucoidan showed only slight focal contraction and moderate vascular meandering (Fig. 3). These results indicate that fucoidan has an inhibitory effect on PVR progression. Therefore, the above suggests that fucoidan may also be used for PVR treatment, and it is expected that fucoidan will also be used in the field of ophthalmology.