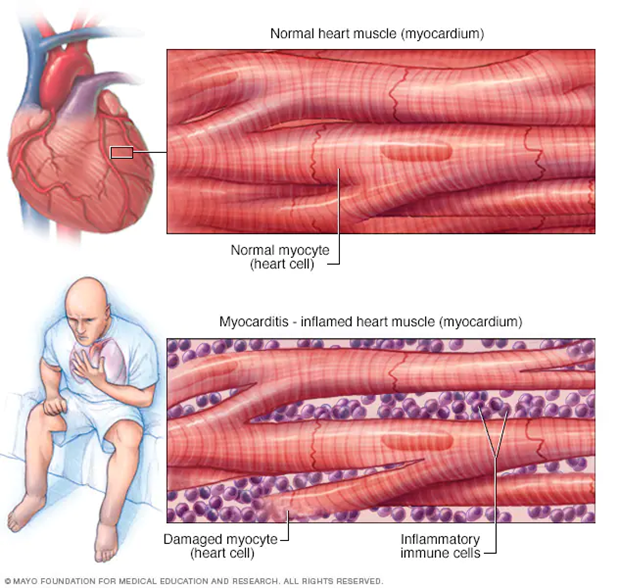
Myocarditis is a condition in which the heart muscle becomes inflamed. It is caused due to viral infection or when a person is already suffering from autoimmune disease. In the case of autoimmune diseases, myocardial myosin is the most abundant of myocardial composition proteins among the 20,000 cardiac-restricted proteins.
The study focuses on myocardial myosin, which is the antigenicity of myosin. The mechanism is that when myocardial myosin-specific CD4-positive T cells return to the myocardium, experimental autoimmune Myocarditis (EAM) is triggered.
Later, neurohumoral factors such as cytokines and chemokines are released in the myocardium, and various bystander inflammatory cells are recruited into the myocardium crossing vascular endothelial cell walls. It causes multiple inflammatory cells to be mobilized across the vascular endothelial cells into the myocardium. Clinical manifestations range from asymptomatic to heart failure, arrhythmias, cardiogenic shock, and might even lead to sudden death.
The effectiveness of immunomodulatory therapies such as steroids and immune globulin has been reported. However, the curable treatment strategy for Myocarditis remains unresolved. On a positive note, Fucoidan, a sulfated polysaccharide, has anti-inflammatory, anti-coagulation, anti-adhesion, anti-tumor, and antiallergic effects. Fucoidan also has revealed the anti-inflammatory effect for ischemic reperfusion myocardial injury and hypoxic-ischemic brie.
So, in this blog, I would like to share a study on the Fucoidan effects concerning Myocarditis that could be related to the Covid-19 vaccine. Therefore I want to discuss Myocarditis to use the study of “Sulfated Polysaccharide Fucoidan Ameliorates Experimental Autoimmune Myocarditis in Rats” by Komei Tanaka et al.
First, seven-week-old male Lewis rats were used and injected myosin from the purified cardiac myosin was extracted from the ventricular muscle of the pig heart. It also included rats undergoing sham surgery or rats with cardiac myosin.
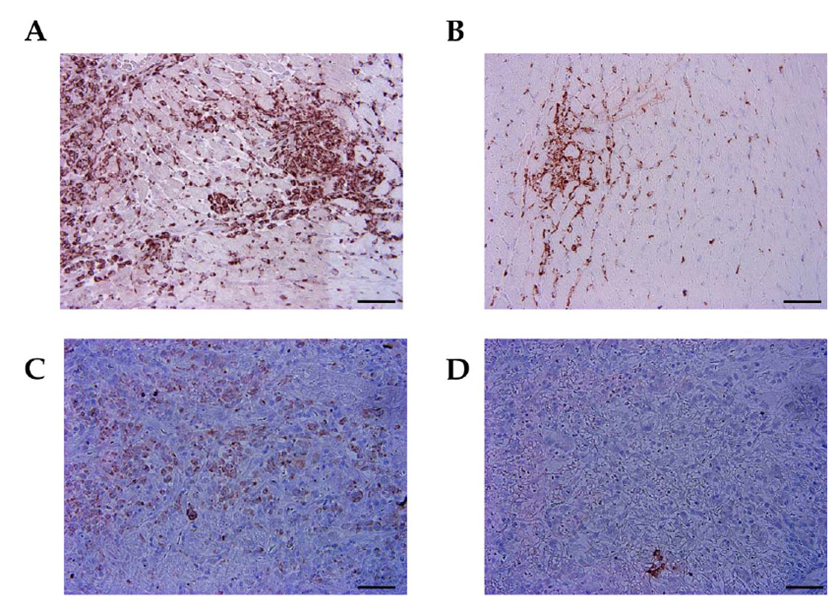
The injection was saline or Fucoidan, and blood pressure and heart rate were measured non-invasively. Thirty-one rats were randomly divided into four groups. Then, Fucoidan was administered at 25 mg/kg per day and observed for 21 days immediately after cardiac myosin injection. The randomly divided rats were observed as follows: Group A – Heart EAM-saline stained with anti-macrophage antibody. Group B – EAM-fucoidan stained with anti-macrophage antibody. Group C – EAM-saline stained with anti-CD4 antibody. Group D – Anti-CD4 antibody EAM fucoidan stained with, measurement of post-hemovascular parameters, rats.
Anesthetized with 2.0% isoflurane in 1.0 L oxygen/min, left ventricular the transthoracic wall assessed (LV) function. As a result, fucoidan treatment for Myocarditis reduced the number of CD4-positive T cell infiltrations in the myocardium (Fig. 1).
Next, the myocardium was infiltrated due to fucoidan treatment to assess changes in inflammatory cells, and immunohistochemical staining was performed using paraffin-embedded sections that searched for heat-induced epitopes in the central ventricle. As a result, The serum TNF-a and IL-6 levels in the EAM-fucoidan group tended to decrease compared with those in the EAM-saline group.
This study demonstrated that fucoidan treatment ameliorated (facilitated) the progression of the rat model of EAM. The beneficial effects of Fucoidan are associated with blocking the transmigration of inflammatory cells into the myocardium and thereby decreasing inflammatory cytokine production.
However, currently, the effects of Fucoidan on ongoing EAM are unclear, so further examination is needed for clinical application.