The development of multiple metabolic diseases is heavily influenced by insulin resistance (IR), which not only contributes to increased morbidity and mortality but also results in significant healthcare expenses. In recent years, there has been a growing focus on deep ocean water (DSW) and fucoidan (FPS) due to their promising potential in the medical and pharmaceutical fields, leading to increased research and exploration in these areas. Hence, in this blog, I would like to share the study, “Combination Treatment of Deep Sea Water and Fucoidan Attenuates High Glucose-Induced Insulin-Resistance in HepG2 Hepatocytes” by Shan He et al. The purpose of the study was to investigate how the utilization of DSW and FPS in combination might ameliorate insulin resistance (IR) in HepG2 hepatocytes that were induced by high glucose concentrations, with a focus on understanding the underlying effects and mechanisms.
While there are numerous antidiabetic drugs currently on the market, it is important to note that the majority of them have been associated with significant side effects and issues with tolerability. In recent times, there has been a growing interest in exploring the potential of various natural products, such as crude extracts derived from natural resources, for treating metabolic diseases. This approach serves as an alternative strategy aimed at developing medicines that are not only more effective but also safer. One such natural product that has gained considerable attention in this regard is Fucoidan.
Deep ocean water (DSW) refers to seawater at a depth of 200 meters or more. DSW, which stands for Deep Sea Water, is not only a safe and stable natural resource but also boasts an unlimited supply, setting it apart from other natural products. This product is rich in minerals, including magnesium (Mg) and calcium (Ca), as well as other beneficial minerals like zinc (Zn), manganese (Mn), vanadium (V), chromium (Cr), and selenium. It also contains trace elements. Additionally, several studies have confirmed that DSW has immune system modulation, antioxidant activity, cardiovascular disease, diabetes, and anti-fatigue effects. The results from both in vivo and in vitro studies demonstrated that his DSW, which had a hardness of 1000 ppm, possesses a range of beneficial properties, including anti-obesity, anti-hyperlipidemic, and anti-diabetic effects. These effects include the inhibition of adipocyte differentiation and lipid accumulation, as well as the improvement of glucose intolerance.
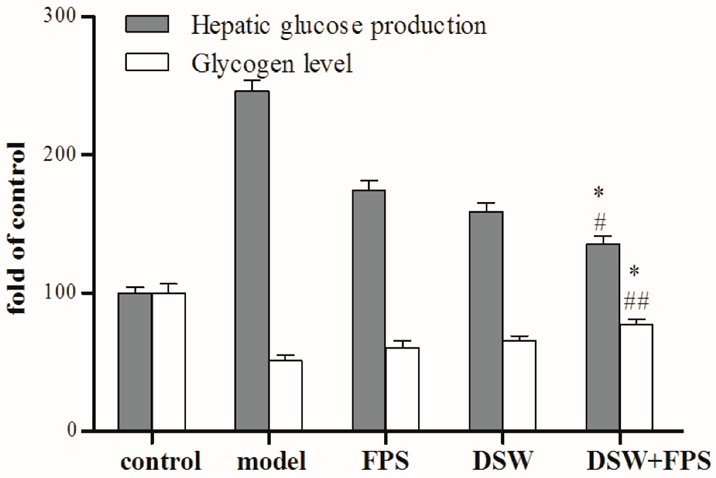
In the initial phase, the combined treatment of DSW and FPS at different concentrations (5, 10, 20, and 50 mg L−1) led to a dose-dependent decrease in hepatic glucose production and an increase in glycogen levels in IR-HepG2 cells. Additionally, when comparing the individual use of DSW or FPS with the combined treatment of DSW and FPS at a dosage of 50 mg L, there was a synergistic effect observed in reducing hepatic glucose production and inhibiting glycogen synthesis in IR-HepG2 cells. (See Figure.1). This study further explained the mechanism of action of the insulin-enhancing effect in IR-HepG2 cells. The findings indicated that the coadministration of DSW and FPS exhibited a synergistic effect on the inhibition of hepatic glucose production and enhancement of glycogen levels in IR-HepG2 cells.
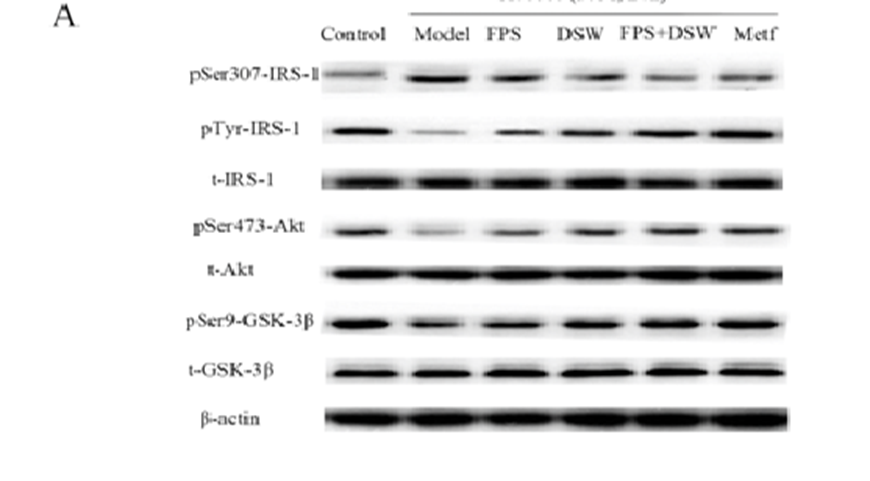
The study aimed to enhance comprehension of the regulatory mechanism involved in the inhibition of hepatic glucose production in IR-HepG2 cells through co-treatment with DSW and FPS. This was accomplished by investigating the expression and phosphorylation levels of insulin signaling pathway components using Western blot analysis. As shown in Figure 2, insulin-induced tyrosine (Tyr) phosphorylation of insulin receptor substrate-1 (IRS-1) occurred normally under glucose treatment at a normal concentration (5.5 mmol L-1). However, under high glucose conditions, Ser 307 phosphorylation of IRS-1 was significantly increased, whereas insulin-stimulated Tyr phosphorylation of IRS-1 was significantly decreased, and insulin-stimulated Ser 473 phosphorylation of Akt was decreased. It led to Ser 9 phosphorylation of glycogen synthase kinase 3β (GSK-3β) in HepG2 cells was also clearly blocked.
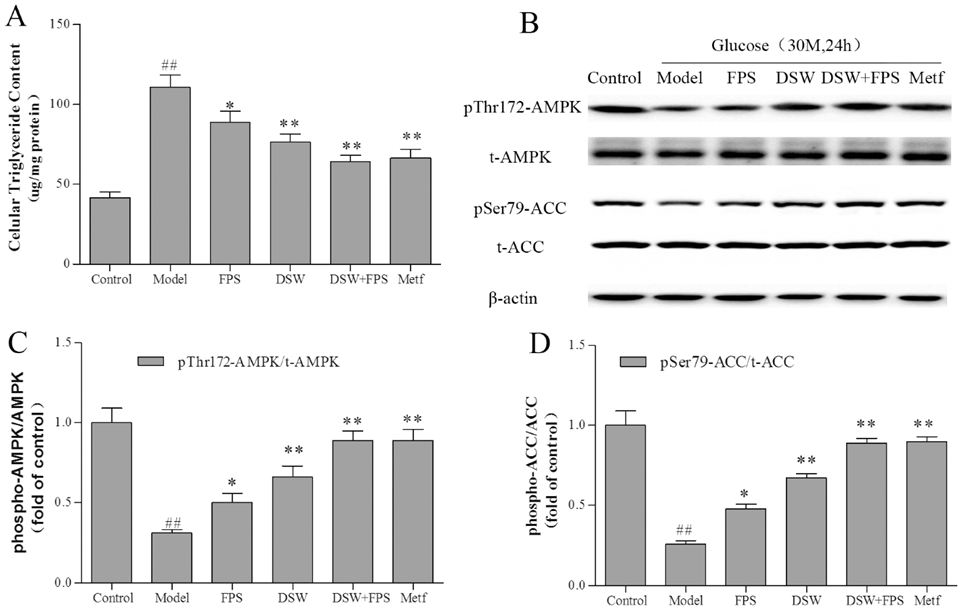
In an effort to enhance their understanding of hepatic lipid metabolism regulation, the researchers chose to investigate how co-treatment of DSW and FPS affects AMPK and its downstream effector ACC, as well as the triglyceride content in HepG2 cells. As shown in Figure 3, exposing HepG2 cells to high glucose (30 mmol L-1, 24 h) decreased the phosphorylation of AMPK and ACC with no obvious changes in total protein levels (Figures 3B-D). In addition to the alterations in AMPK and ACC phosphorylation, there was a substantial rise in triglyceride content, reaching almost three times the initial amount in IR hepatocytes, as depicted in Figure 3A. On the other hand, when DSW and FPS were administered together, there was a significant increase in the phosphorylation levels of AMPK and ACC. In addition, intracellular triglyceride content was also reduced by 40%.
In conclusion, when considering the results as a whole, it can be inferred that the combined use of DSW and FPS had a more significant positive impact on insulin resistance (IR) compared to using DSW or FPS individually. They may attenuate IR by targeting Akt/GSK-3β and AMPK pathways. These findings may have significant implications for the way metabolic diseases are treated.
Source: Mar. Drugs 2018, 16(2), 48; https://doi.org/10.3390/md16020048
